Calderdale NHS has stumbled further down the stealth privatisation road by awarding a 12 month, £364K contract for telehealth and telecare to Tunstall Healthcare, a company largely owned by vulture fund Charterhouse Capital Partners.
Private equity company Bridgepoint sold Tunstall to Charterhouse in 2008 for more than double the £225m it paid for it in 2005. Bridgepoint, which acquired Care UK in early 2010 for £423m, retains a minority share in Tunstall.
A Freedom of Information (FOI) request has shown that the NHS Calderdale telehealth/telecare contract with Tunstall Healthcare, launched in July 2013, is being rolled out in two phases, as part of a wider “Quest for Quality in Care Homes” initiative. The reply to Upper Calder Valley Plain Speaker’s FOI request states:
“Phase one is focusing on providing telecare solutions for up to 400 residents within 25 nursing and residential homes in Calderdale. Phase two will enable a further 500 residents in care homes to benefit from telehealth solutions (telemonitoring) in 2014.”
According to Tunstall Healthcare, the Quality in Care Homes contract includes the UK’s largest procurement of telehealth and telecare gadgets for care homes.
Evaluation and recommendations on the bid were not presented to the Calderdale Clinical Commissioning Executive
Tunstall’s teleheath and telecare contract for Calderdale care homes, publicly announced in July, was awarded in February 2013 by the NHS Calderdale, Kirklees and Wakefield District Cluster.
The contract was not publicly advertised – only three telehealth and telecare providers listed in the Government Procurement Services Framework RM784 had been invited to bid. This didn’t go down well with some members of the Procurement Committee, and it seems to have been a rushed job. The Procurement Committee minutes record that
“the evaluation and recommendations had not been presented to the Calderdale Clinical Commissioning Executive due to timescale.”
Use of the passive voice (“had not been presented”) makes it impossible to grasp whose failure that was.
Delivering “efficiency savings” in end of life care – where’s the evidence?
In addition to the “assistive technology” contract awarded to Tunstall Healthcare, the Quality in Care Homes initiative includes the establishment of a Multi Disciplinary Team (MDT) for care homes. The £1,055,000 MDT contract was advertised on the supply2health website and awarded on 22nd October 2013, under the Any Qualified Provider rules.
Upper Calder Valley Plain Speaker has found that Calderdale Clinical Commissioning Group (CCG) awarded the MDT contract to Calderdale and Huddersfield Foundation Trust (CHFT), following an “Open” procurement where all tenders received from interested parties were evaluated. Details of the process and outcome are set out in a paper submitted to the Calderdale CCG Governing Body meeting in November.
At least the MDT element of the Quest for Quality in Care Homes contract has gone to the NHS, not to a private company.
The supply2health ad states that a key function of the multi-disciplinary team is to manage end of life care with the use of assistive technology, calling in GPs as necessary.
In 2012 the British Geriatrics Society advocated setting up multidisciplinary teams in care homes to make sure that appropriate healthcare is available for care home residents, who often have many long term health problems.
Tunstall Healthcare states that the
“multi-disciplinary team…will be available to support and advise staff in care homes on the prevention and proactive management of the needs of older people, including fall prevention and medication management.”
Upper Calder Valley Plain Speaker asked Calderdale Clinical Commissioning Group (CCG) for the clinical evidence and full business assessment for the Quality in Care Homes scheme.
On behalf of Calderdale CCG, West and South York Yorkshire and Bassetlaw Commissioning Support Unit replied:
‘The focus of the project is not on supporting the discharge of individuals from A&E. The main aim of the MDT project as set out in the specification is: “To commission a Multi-Disciplinary Team(s) to support homes to effectively manage individuals, avoid unnecessary admissions, reduce the demand on General Practice by providing planned and proactive care, support timely, safe and sustainable discharges and enable patients to die in their place of choice”.
One of the key elements of the project, as stated in the attached paper, will be to evaluate the quality and quantify the impact made against the key result areas in the specification.
A formal review of the service will be undertaken on a 3 monthly basis to determine outcomes and discuss the development of the project.’
National trial concluded telehealth is not cost-effective addition to standard care
In 2012, the BMJ reported on the most recent evidence from the NHS Whole System Demonstrator (WSD) trial. This is the biggest and most comprehensive investigation of telehealth and telecare conducted in the UK . The most recent evidence shows no generally significant difference in emergency hospital visits for home-based patients in telehealth pilots and patients receiving traditional care.
This research did show that telehealth pilots were associated with lower mortality and fewer hospital admissions during a 12 month follow up, than for patients with similar illnesses who only received traditional care. But the researchers note that the trial recruitment process could have affected the results of the trial, and that the difference in hospital admissions was small,
“raising questions about the clinical relevance of the results”.
A March 2013 study of the cost effectiveness of telehealth for patients with long term conditions, published in the British Medical Journal, found that the benefit to patients of telehealthcare plus usual care was similar to that for patients receiving usual care only, and total costs associated with the telehealth care were higher. The study concluded,
“Telehealth does not seem to be a cost effective addition to standard support and treatment.”
Calderdale Council’s Cabinet Member for Adults, Health and Social Care, Councillor Bob Metcalfe said,
“I am committed in helping to ensure there is an increase in the level of support and quality of care in Calderdale’s Care Homes. The introduction of telehealth and telecare is just one important strand of how we are working with health colleagues to improve this quality of care.
I am unable within the time available to comment further on the ‘context’ of your article. (I would mention that a Calderdale and Huddersfield NHS Foundation Trust membership councillor is of course a different role and responsibility than that of a CHFT Board member.)”
Tunstall Healthcare – a profit machine for private equity companies
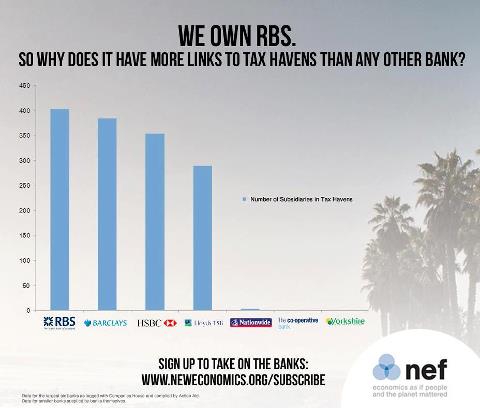
Charterhouse Capital Partners bought Tunstall Healthcare for £510m in March 2008, funded with £237m debt from the Royal Bank of Scotland (RBS), six months before RBS went bust as a result of bad decisions and lack of due diligence in its investment banking arm.
RBS was bailed out with £45bn of taxpayers’ money pumped directly into the bank and several hundred billion pounds more provided in loans and guarantees. Our public money also indirectly served to bail out companies like Charterhouse Capital Partners that RBS had invested in.
Bridgepoint’s profit on the sale of Tunstall Healthcare to Charterhouse Capital partners was around £280m – much of it from public funding via NHS and local authority purchases of Tunstall Healthcare equipment.
Think what NHS and local government services those hundreds of millions of pounds could have paid for.
If you don’t want to see public funding turned into private profit, you might like to make your views known to Dr Alan Brook, Chair of Calderdale Clinical Commissioning Group, and to Calderdale Council’s Cabinet Member for Adults, Health and Social Care, Cllr Bob Metcalfe. Not to mention Calderdale MP Craig Whittaker. (I can’t find any contact details for Dr Brook apart from the contact form for Longroyde Surgery in Rastrick, where he works.)
A Tunstall Healthcare press release quotes Cllr Metcalfe as saying,
“Calderdale Council is very pleased and committed to be working in this partnership to provide more personal safeguarding and reassurance for both care residents and their families, with the introduction of telecare and telehealth in local care homes.”
Like other companies that are indebted to private equity companies, Tunstall Healthcare has to make massive interest payments on its debt to Charterhouse Capital Partners and others.
Accounts for 2008-9, the year after Charterhouse Capital Partners bought the company, show that Tunstall Group’s global companies were laden with £607.2m of debt. Its interest payments on the debt cost £87.5m.
As a result, the global Tunstall Group made a loss of £84.1m on a worldwide turnover of £141.7m – although Tunstall UK did well, making a profit of £28.7m before tax on a turnover of £86.4m.
Public funding for private profits
Tunstall UK made these 2008-2009 profits on the back of sales of telehealth and telecare products to local authorities and the NHS – much of it funded by the Department of Health’s Preventive Technology Grant and its investment in the Whole System Demonstrator Programme.
From 2006-2008, the UK government’s Preventive Technology Grant (PTG) provided £80m for local authorities to kickstart their purchase of telehealth and telecare for older people living at home and in sheltered housing. The aim was to provide at least 160,000 older people with telehealth or telecare equipment.
From 2008-2010, the UK government invested £31m in the Whole System Demonstrator Programme. This funded telehealth and telecare demonstration projects in 230 GP practices in three areas of England, involving 6,000 patients at risk of hospital admission because of heart failure, COPD or diabetes, and adults with social care needs.
A good slice of this £31m will have gone to Tunstall: the company supplied telecare products to all three areas that took part in the Whole System Demonstrator programme, and telehealth products to one of the areas.
When Charterhouse Capital Partners acquired the company, Tunstall Healthcare was about to benefit from the Department of Health investment in the Whole System Demonstrator, and already had an unusually close relationship with the Department of Health.
One of only six listed suppliers that are recommended for all categories of telehealth and telecare products and services in the Government Buying Solutions Framework, Tunstall Healthcare was already one of the main telecare and telehealth providers for local authorities and the NHS.
Private equity companies like Bridgepoint that want to profit from the sale of their equity have form in getting the companies they hold equity in to bid for government contracts, just before they sell them. A guaranteed income stream from the government increases the sales value of the company.
Opening up the NHS to this kind of profiteering is,
“ a reckless gamble with people’s health. In the long run, it will give us something close to the most expensive and worst health system in the developed world, that of the USA…For the private sector it will be the bonanza that its spokesmen have openly campaigned for.” (Colin Leys & Stewart Player, The Plot Against the NHS, p 143)
After the Preventive Technology Grant ended, the Tunstall Group’s 2009-10 UK revenues fell seven per cent to £66.7m.
According to a local authority telecare coordinator, the slump in telecare and telehealth sales following the end of the Preventive Technology Grant was predictable. The Preventive Technology Grant was largely driven by
“the industry’s need to sell as much equipment as possible”
As a result, local authorities found themselves with
“a stash of equipment that nobody wants”
The local authority telecare coordinator reckoned that this could create a local authority backlash against buying telecare and telehealth kit.
Tunstall CEO calls on government to encourage NHS and local councils to buy their products
As Tunstall’s UK sales fell dramatically, in July 2009 Tunstall Healthcare CEO James Buckley announced he was planning to cut up to 70 of the 550 UK staff. He called on the government to do more to encourage local councils and primary care trusts to install systems like Tunstall’s.
By the end of 2009, Tunstall Healthcare’s order book had recovered. A recruitment company advertised on their behalf:
“Our client is the market leader in Telecare and TeleHealthcare solutions… Due to an increase in demand within the market place our client is now looking to bolster their client support resources…”
Ta da! £millions result for Tunstall in North Yorkshire – but audit says Tunstall contract unjustified
In September 2009 North Yorkshire and York Primary Care Trust (NYYPCT), the largest PCT in England, had started a £300,000 trial of 120 Tunstall telehealth units to remotely monitor patients with Chronic Obstructive Pulmonary Disease (COPD). The trial was due for evaluation in April/May 2010.
In October/November 2009, well before their telehealth trial was completed – much less evaluated – NYY PCT made preparations for an additional £3.2m procurement of 2,000 more Tunstall gadgets.
Telehealth and Telecare Aware reported that in mid December 2009 North Yorkshire & York Primary Care Trust had issued the invitation to tender without openly advertising, using the old PASA Telecare National Framework Agreement.
This Framework Agreement was the forerunner of the Government Procurement Services Framework RM784 that the NHS Calderdale, Kirklees and Wakefield District Cluster has used to procure Tunstall telehealth and telecare kit for Calderdale Care Homes and home based patients with COPD.
Three companies submitted tenders for the NYYPCT stage 2 contract. Without requiring a business assessment, the £3.2 million procurement was completed in March 2010. Two thirds were funded by the Strategic Health Authority, the rest by the NYY PCT. Telecare Aware reported that £1m out of the £3.2m went to project consultants Ernst & Young.
Telehealth and Telecare Aware also reported,
“In addition to the upfront cost, the PCT committed to paying a substantial sum [believed to be in the order of £500,000] in annual maintenance and other charges.”
At the time, the NYY PCT was heading for an annual deficit of £8m. The Chief Executive of NHS NYY said that they were looking to make savings through the telehealth trial.
In August, NYY PCT Director of Strategy David Cockayne jumped ship and started working as Tunstall’s healthcare strategy director in October 2010. By then only 135 of the 2,000 telehealthcare units were in use.
York GP and vice-chairman of the Local Medical Committee, Dr Brian McGregor, was asking why the primary care trust, with a £23 million deficit, had invested £3.2 million on a system that was still being trialled.
Good question.
Cockayne was the second public servant responsible for commissioning £millions of Tunstall kit to spin swiftly through the revolving door into Tunstall employment. He followed David Kelly, who moved to Tunstall from the West Lothian Community Health and Care Partnership where he had overseen a £1m trial of Tunstall telehealth equipment.
15 months later, in January 2012, the Yorkshire Post reported that it had seen an internal audit report by North Yorkshire and York Primary Care Trust (PCT) that failed to find any evidence to justify the scale of the telehealthcare project.
Only around a fifth of the 2,000 units had been used, making a mockery of NYY PCT hopes that telehealthcare for patients with COPD, heart failure and diabetes would significantly cut hospital admissions and save the NHS £3.4m by March 2011.
By June 2011 less than £200,000 had been saved. The unused telehealthcare kit was sitting in a bonded warehouse. NYY PCT had resorted to paying GPs to get them to prescribe the telehealth kit for their patients.
The internal audit also criticised the procurement process, since there was no evidence or business case to justify the investment in the 2,000 unit. It said that in future, procurement should involve full business assessments for major projects.
A doctor at Cotswald Medical Practice commented on similarities with a £5m procurement of 2,000 Tunstalls Healthcare devices in Gloucester – again project managed by Ernst & Young.
The Gloucester doctor said the telehealthcare scheme been imposed on GPs without any consultation, and most patients whom the Practice had identified as suitable for using the telehealthcare kit did not want it.
Hopefully these experiences will not be repeated in Calderdale.
Perhaps the move into Care Homes is a result of the failure of Tunstall Healthcare initiatives for patients based at home?
More here on Tunstall Healthcare’s spin, lobbying and support for the Coalition goverment’s NHS land grab.
Updated 28/12/2013 with information from the Quality in Care Homes Freedom Of Information reply