The NHS competition enforcer David Bennett has told NHS Foundation Trusts that if they don’t bring down their deficits, they will lose their freedom to decide their own strategy and the way they run their services. This includes the power to retain their surpluses and borrow to invest in services for patients.
The 152 foundation trusts together face a £1bn deficit this year, but the government has decided this is “unaffordable”.
David Bennett, the Monitor boss, told NHS finance directors they have to bring this deficit down by speeding up productivity improvements and working in new ways.
He told the annual conference of the Healthcare Financial Management Association (HFMA):
“Current plans are unaffordable, and all providers have to make a major contribution to efficiency improvements, even those who aren’t currently forecasting to be in deficit. This means hospitals leaving no stone unturned, and adopting best and better practice everywhere; avoiding unnecessary expenditure, and adopting new ways of working.”
But Calderdale and Huddersfield NHS Foundation Trust is in deficit because it could not make last year’s required £20m “efficiency savings” without damaging patient safety, and as Calderdale Clinical Commissioning Group (CCG) told Calderdale Council Adults Health & Social Care Scrutiny Panel, it would not allow the Trust to make cuts that would damage patient safety.
Cutting hospital services so neighbouring “providers” can supply them instead
David Bennett told the HFMA conference that individual foundation trusts may need to cut services so that neighbouring hospitals and providers can provide them instead.
He said:
“We want to work with you to redesign patient services across organisational boundaries, where there may be some winners and some losers. We are not advocating the closure of vital hospital services, but we recognise that in some places they can be run better on a shared basis by trusts within a geographical area, for example through clinical networking arrangements.”
In 2013 Jeremy Hunt tried to force this on South London hospitals when the debt-burdened South London Healthcare Trust went into deficit, burdened by massive Private Finance Initiative debts. It was taken over by a Trust Special Administrator (TSA), who ordered cuts and closures at the neighbouring Lewisham Hospital in order to protect the South London Healthcare Trust’s PFI debt repayments.
The Save Lewisham Hospital campaign twice fought the TSA’s proposed cuts and closures in court, and won. The Tory government then changed the law to make sure that Trust Special Administrators could not be challenged in future if they tell hospitals to give up “the provision of some medical specialities to others.”
Hospital chains – like Academy chains?
At the Healthcare Finance Management Association conference, the Monitor boss backed foundation trusts that were willing to take over the running of others in difficulty, leading to the establishment of “successful chains of hospitals”.
He said Monitor would get the best performers to help the poorest through buddying arrangements, and create a pool of troubleshooters to turnaround struggling trusts.
This all sounds very much like the programme of turning local authority schools into academy chains. A recipe for privatisation, profiteering and generally dismal standards.
“Buddying arrangements” and the Monitor boss’s other proposals are based on the Dalton Review, which last year suggested companies could be contracted to manage publicly funded hospitals, among other commercial measures. The Dalton Review Panel included panel of executives including Steve Melton, the boss of private healthcare company Circle and previously Argos supply chain director. Jim Easton of Care UK was also one of the Dalton Review panel’s experts and the National Health Action Party reports that an FOI request shows that he was representing the main private sector lobby group.
Monitor has already imposed central controls on foundation trust spending, like agency staffing and management consultancy. And Bennett warned that Monitor would act sooner over under-performance and demand faster responses.
Trusts found in breach of their licence would be ranked according to the seriousness of their financial and operational problems, echoing the Special Measures regime for inadequate care.
Monitor has already imposed enforcement undertakings on Calderdale and Huddersfield NHS Foundation Trust for breaching its licence conditions, through its failure to make massive government-required cuts, because this would have endangered patient safety.
Dr Bennett said:
“The Five Year Forward View sets out a vision for how the NHS needs to change but it is going to be hard work getting there, especially as we have a huge challenge on our hands right now.”
He added:
“I recognise that just because deficits mostly sit with providers doesn’t mean they are the only NHS organisations that need to up their game.”
Acknowledging that the NHS payment system had put the onus on providers to make efficiencies in the past, Dr Bennett signalled that commissioners would have to play an increasing part by “managing demand” and redesigning services.
Despite the brilliant success of the Save Lewisham Hospital campaign, they fear revived plans to close Lewisham Hospital and sell off its site, that have appeared in the latest South East London healthcare strategy document.
They say that these arguments for reconfiguring NHS services in south east London are very similar to those used by the Trust Special Administrator in 2012. They are also very similar to the Right Care Right Time Right Place changes that Clinical Commissioning Groups in Calderdale and Kirklees are weaselling through, having shied away from the scheduled public consultation that should have taken place last autumn.
You can sign Save Lewisham Hospital’s new petition here.
With the government’s ideologically-driven funding stranglehold on the NHS, a divide and rule strategy is at play
Chris Hopson, chief executive of NHS Providers, said in response to David Bennett’s speech:
“Whatever is decided and however great the pressure, we need to resist the temptation to think that these issues are best addressed by reverting to command and control and eroding provider freedoms. The way to meet this challenge is to enable, support and empower providers, rather than threatening or neutering them.”
The Kings Fund warned, ahead of the 8 July Budget, that unless the government finds additional funding:
“a growing black hole in NHS finances could have significant consequences for patient care.”
Local NHS, Council and third sector companies at each others’ throats
Calderdale Clinical Commissioning Group and Calderdale and Huddersfield NHS Foundation Trust (the hospitals Trust) have still not agreed the 2015-16 contract, which should have started on April 1st. Their dispute has recently gone to arbitration, since they’ve been unable to resolve it even after months of wrangling.
Locala has made a legal challenge to Kirklees Council over the Council’s award of the £3.5m integrated sexual health services contract to the hospitals Trust, so Kirklees Council has been unable to award the contract although it made the decision in April.
Greater Huddersfield and N Kirklees Clinical Commissioning Groups (CCGs) have been unable to award the £283m Care Closer to Home contract because the unsuccessful bidder (Calderdale and Huudersfield NHS Foundation Trust) has raised “concerns” about the CCGs’ decision in mid-May to award the contract to Locala. Unconfirmed rumours are now circulating that the hospital Trust’s “concerns” have escalated to a legal challenge, which I am trying to establish the truth about.
And the CCGs plough on with the intention of wreaking further “transformation” on our NHS and social care services. A pointless Calderdale public consultation is due in the autumn on cuts and closures to our hospitals. This meaningless consultation is apparently unlawful, because the future of the hospital will already have been determined by decisions to move many services out of Calderdale Royal Hospital into the community.
Meanwhile Caroline Lucas MP and 11 other cross-party MPs have responded to this deliberately engineered, top-down mess of marketisation and privatisation, by presenting the NHS Reinstatement Bill for its first House of Commons reading on July 1st. This Bill would restore the NHS to full public ownership and rational, fair planning and allocation of resources, to meet the needs of patients not profiteers. Please ask your MP to vote for it.
Monitor and other regulators have new legal duty to promote economic growth and put commercial interests first
Since the 2015 Deregulation Bill became law, regulators such as Monitor:
“…must…have regard to the desirability of promotiong economic growth”.
And they must “exercise the regulatory function” in ways that promote economic growth. (Clause 103)
Doesn’t this create an ethical conflict when government-appointed regulatory bodies have a legal duty to put commercial gain above other factors like protection of the public and our interests?
Perhaps not for David Bennett, the Monitor boss who was previously a Senior Partner at McKinsey, the management consultancy company that’s made a killing out of the corporate capture of the NHS under both the New Labour and Coalition governments.
The Kings Fund warned, ahead of the 8 July Budget, that unless the government finds additional funding:
“a growing black hole in NHS finances could have significant consequences for patient care.”

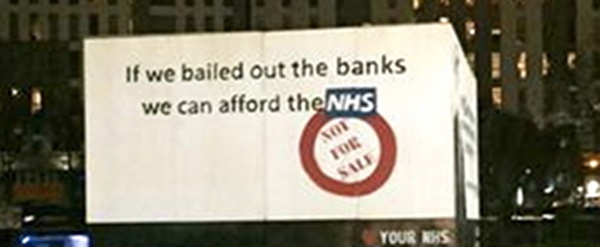
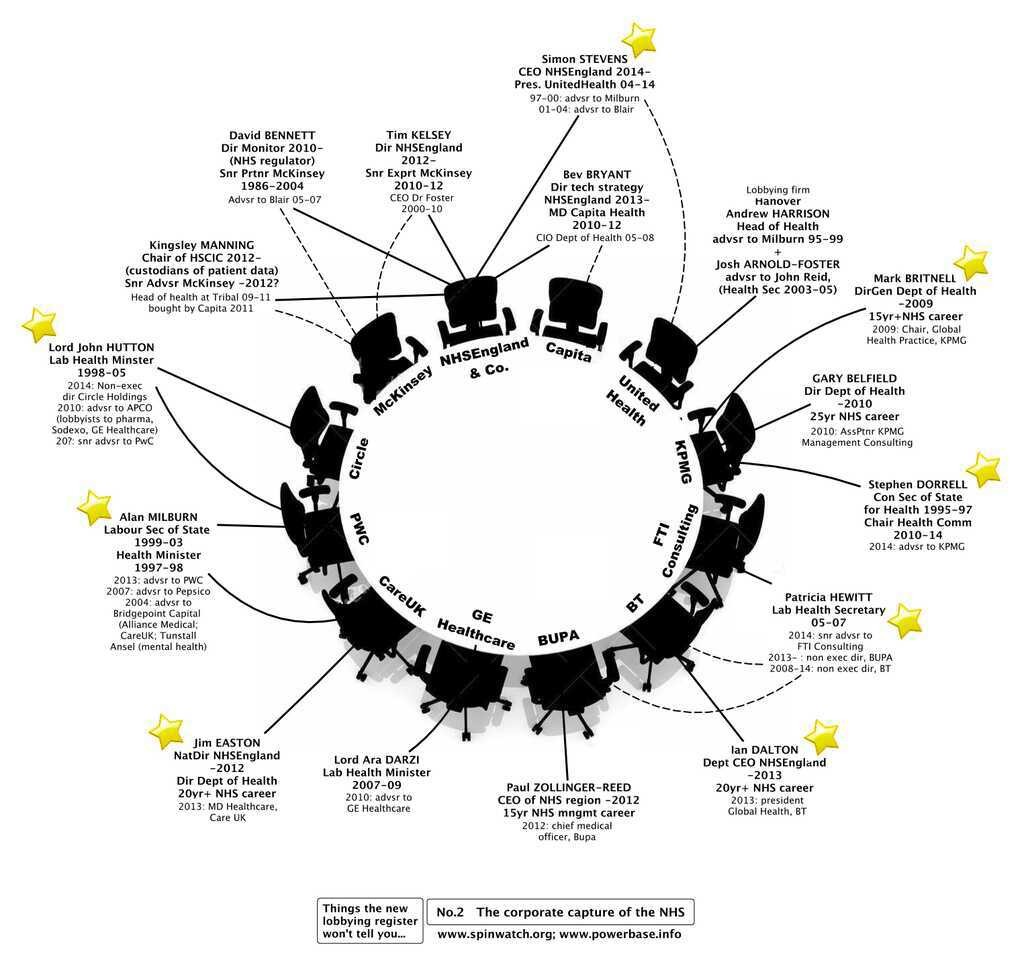
Get rid of the internal market commissioning process. That is the answer. The missing money is all there. It’s being spent on setting up contracts, evaluating tenders, monitoring contracts, employing lawyers to check competition rules, armies of accountants and development officers and breathtakingly expensive consultancy companies. And paying the Commissioning Support Units millions to break up the NHS and hand it out to companies that are in competition with each other. How is that any good for our health and what an obscene waste of public money.