People are rightly very exercised about the proposed hospital cuts and A&E closure – but the proposals to move hospital services into the “community” are equally devastating.
This bit of the “Right Care Right Place Right Time” shake up – which should really be called “Less Care, Fragmented Hither and Yon” – has the potential to wreak destruction on the bit of the NHS that most of us use more than anything else – our GP/primary care services.
This is Part 2 of Plain Speaker’s attempt to begin to answer some key questions about so-called Care Closer to Home. (You can find Part 1 here)
There is no real evidence that “Care Closer to Home” will serve its stated purpose of reducing emergency hospital admissions of patients with Ambulatory Care Sensitive Conditions conditions (ie cardiovascular and respiratory ailments) and patients with Conditions Not Requiring Admission – mostly frail elderly people’s illnesses and children’s “complex needs”.
What follows is based on information drawn from the Right Care Right Time Right Place Pre Consultation Business Case (PCBC) – and from other sources, as the PCBC is full of holes .
It deals with these questions:
- Which services would be moved out of hospitals into the “community”?
- What evidence is there that Care Closer to Home will do what it says on the tin? (Spoiler alert: Next to none.)
- Where in the community would these services go?
- How would these services work in the community?
- What is Patients’ Self care all about?
Which services do they want to move of the hospitals into “the community”?
Calderdale
Hospital services that Calderdale Care Closer to Home (CC2H) Phase 2 wants to move into the community are those that care for people with Ambulatory Care Sensitive Conditions (in other words, people going to A&E because of illnesses and frailty that wouldn’t have got so bad if they’d been better looked after) and CNRA- Conditions Not Requiring Admission.
To reduce emergency hospital admissions of patients with Ambulatory Care Sensitive Conditions conditions, the focus is on:
- Respiratory and Cardio vascular disease.
To reduce emergency hospital admissions of patients with Conditions Not Requiring Admissions, the focus is on:
- frail elderly illnesses: flu, pneumonia, UTI, dehydration, gastroenteritis, which also apply in smaller numbers to children and young people
- children with complex needs and their parents
Under those 2 categories, these are the specific services that Calderdale CCG is considering moving out of the hospital into the “community”, on the basis of “assumptions” the CCGs have “created” with their “providers” (Pre Consultation Business Case p 46):
- Respiratory (children and adults)
- Frailty – falls, Urinary Tract Infections and Care Homes
- Cardio Vascular Disease
- Diabetes
- MSK (ie muscular skeletal disorders)
- Opthamology
- Dermatology
- Diagnostics (Vanguard)
- Ear Nose & Throat (ENT)
- End of Life Care
- Rehab Bed Days
Many of these are planned care services – so, how many of the planned care services will actually end up in the new 119-bed Huddersfield planned care clinic?
Huddersfield
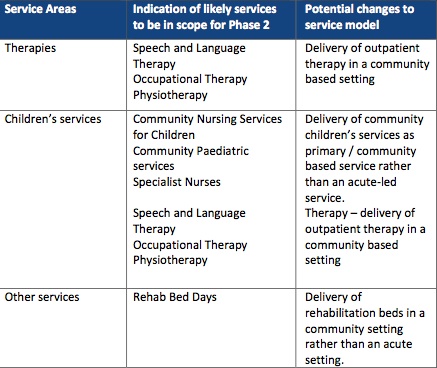
The Pre Consultation Business Case says that for Greater Huddersfield Clinical Commissioning Group’s (CCG’s) Phase 2 Care Closer to Home, the services it is considering moving fully or partly out of hospital are:
No real evidence that Care Closer to Home will do what it says on the tin
There is little or no evidence to support the assumption that moving services out of the hospitals into the Care Closer to Home scheme will reduce avoidable acute and emergency hospital admissions.
A Nuffield Trust briefing (NHS hospitals under pressure: trends in acute activity up to 2022) said that plans to replace acute and emergency hospital services by care in the community are not likely to work, given the evidence that:
“To date, attempts to reduce the numbers of people admitted to hospital through better preventative care in their communities have not been very successful on a large scale” ( p2)
“Current policy is aimed at cutting the number of emergency admissions by providing more, better services outside hospital that can either prevent the need for hospital admission or offer the same care but in different settings. This is a common theme in initiatives for more integrated services, including the government’s Better Care Fund. But there is little evidence that this can be achieved.(Bardsley and others, 2013).” (p11)
Reporting on its Commission on Hospital Care for Frail Older People, the Health Service Journal (November 2014) stated:
“There is a myth that providing more and better care for frail older people in the community, increasing integration between health and social care services and pooling health and social care budgets will lead to significant, cashable financial savings in the acute hospital sector and across health economies. The commission found no evidence that these assumptions are true.”
A 2014 review of the evidence for promoting integrated care, published in the Health Services Journal, found that:
“a close look at the data highlights a dearth of evidence on the impact of integrated care”.
This is a 2014 review of the Right Care Right Time Right Place proposal to move services out of the hospitals, published in OurNHS.
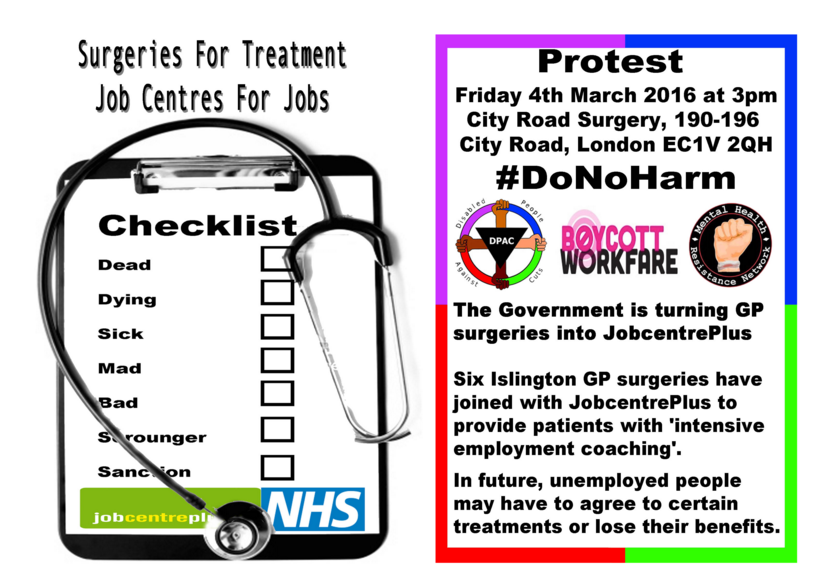
Social care has been plagued for decades by cuts, outsourcing and piecemeal privatisation of services, leaving many staff on zero hour contracts and service users with 15 minutes sessions of care. There are very real fears that the integration of health and social care will mean the plundering of already inadequate NHS budgets to prop up local government services.
The danger is that under local authority rules, integrated health and social care will mean that there will be means-tested charges for services rather than the NHS principle of services funded from general taxation. The outcome may be a devolved, deregulated, local service, partly privatised, its social care component already 90% privatised, facing a meltdown in local authority finance, competing with other localities for patients and funds, with local pay and conditions for health workers, and all branded as “integrated”.
Where in the community do they want to put these services?
The Pre Consultation Business Case is a bit vague about this, but the Calderdale CCG Care Closer to Home section (4.3) mentions upgraded premises and
“…developing plans to maximise our use of community estate” (p46).
(This is about trying to make the white elephant Todmorden Health Centre – which was built as a Darzi clinic – pay its way).
It also mentions “making better use of community facilities”, (p42) so that:
“primary and community care staff will also work closely with secondary care and social services through some of the models outlined in the NHS Five Year Forward View” (p 42).
A recent Greater Huddersfield Clinical Commissioning Group Governing Body meeting approved a plan to close 4 GP practices in Huddersfield and replace them with a new-build Primary/Community Care “hub” on the old Kirklees College site, that would have 10K patients. This is part of a national trend to move towards huge GP practices run by private companies.
Calderdale Care Closer to Home Phase 2 aims to keep patients at home, out of hospital, for as long as possible, and if they have to go to hospital, to discharge them as soon as possible. (Pre-Consultation Business Case, p52)
This is how they aim to cut hospital costs.
Although the costs of providing decent community/home-based care are high. So if they were to do it right, it probably wouldn’t save money.
And as mentioned in Care Closer to Home: “Patients Will Suffer: (part 1), on p 136 of the Pre Consultation Business Case, the Clinical Senate says that that the Community Services Specifications for Calderdale, Greater Huddersfield and North Kirklees CCGs lack information about
“whether the care closer to home vision is achievable financially”.
Greater Huddersfield CCG Care Closer to Home – Plans and Phase 2 (Pre Consultation Business Case p 49) says they are planning to make £2m cash releasing “efficiency savings” (ie cut spending on some things by £2m/year, so that £2m extra dosh is available for something else) – and it will take 4 years to achieve this.
How will these services work in the community? (The Clinical Senate says it can’t tell )
There will be a:
“new integrated community model…delivering care out in the community wherever possible”. (Pre Consultation Business Case p45)
This would bring together: health care,social care, primary care and third sector support – including new models of community-based:
- urgent care,
- end of life care,
- planned care eg MSK (musculoskeletal), ophthamology, dermatology and END [?] and care provided in care homes)
On p 139 of the Pre Consultation Business Case, the Clinical Senate notes that the CCGs have not worked out how to avoid “fractured delivery of care to patients”, given the complex integrated system, and that the CCGs are planning to commission a lead provider for their Care Closer to Home schemes.
This means that one provider would get the contract and then subcontract it out to multiple other agencies. (see Care Closer to Home Part 3 – coming shortly – Who would run this “new integrated community model”?)
The Clinical Senate say that the Care Closer to Home scheme won’t work unless GPs support it. Which is a bit of a no-brainer, so why mention it?
It seems from the Clinical Senate’s comments that this support may not be forthcoming, because apparently “in the consultation” (what consultation? We haven’t had the consultation yet) the “view was expressed” (who by? Presumably by GPs – why does the Clinical Senate write so opaquely? Don’t they dare to speak out?) that “one size doesn’t fit all.”
But, as the Clinical Senate points out, for the Care Closer to Home model to work, one size hubs have to fit all, so that there can be
“consistent signposting and referral of patients”
– the clear implication being that otherwise patients will be lost in a maze of fragmented services providing by a slew of subcontractors each with a little bit of the action handed out to them by the “lead provider”.
The Clinical Senate also had a few things to say about the CCGs’ plans for moving end of life care into the community and having palliative care principally delivered in the community (Pre Consultation Business Case on p71).
It found that the Care Closer to Home specifications were unclear about the role and responsibility of the end of life care coordinator and about the processes of delivering end of life care in the community.
And the specifications made no mention of consultant geriatric provision, but the difficulties in recruiting consultants will potentially pose a risk to the service
(p 140).
What if people have nowhere out of the hospital to go and be cared for while they die?
A friend of mine says if it gets to that stage, she and her partner plan to go up on the tops, pitch their tent and wait for hypothermia to do the job.
The Clinical Senate say they can’t certify that the proposed community services specifications would generate the required quality of care.
This is because the Community Services Specifications’ “visionary style” hampered their efforts to review the proposed functions and capacity of the new system and the risks associated with the service transformation.
Greater Huddersfield CCG’s already set up Care Closer to Home Phase 1 “model” (Pre Consultation Business Case p 47) includes:
- risk assessment to identify patients who are most likely to be admitted to hospital
info to help people self-care (this involves trawling through patients’ confidential medical records, although the Pre Consultation Business Case doesn’t say this) - single point of contact for patients, carers and staff
- “integrated multi-professional locality teams working closely with general practice”
- urgent teams for rapid response within 2 hours
- routine teams for routine stuff
- specialist expert teams eg long term conditions management, tissue viability [??? is this bedsores? An online search reveals that tissue viability is “wound prevention and management” and what they call “pressure ulcers” seems like a big part of it] and mental health
- planned services eg dermatology MSK delivered through clinics
- digitech
But the Clinical Senate says (Pre Consultation Business Case p141) that Greater Huddersfield CCG’s Care Closer to Home document omits information about:
- “the level of health knowledge available in the triage process” – this process is where patient calls go to a Single Point of Access and are then transferred to an Access and Coordination Hub within each “locality”. [Sounds like a potential rerun of NHS 111 problems?]
- what is meant by “therapist” in the rapid response function and how commissioners are going to deal with shortages of specific therapy skills
- how mental health teams will work with Care Closer to Home services and make use of the access and co-ordination hubs
- how hubs link with mental health single point of access
- lack of information about the numbers of specialist staff that will be available to support patient care closer to home and how this relates to staff who currently work “in the system”
The Calderdale Care Closer to Home Phase 2 model (Pre Consultation Business Case p 44) is laid out differently from Greater Huddersfield’s but boils down to much the same things.
Greater Huddersfield CCG’s new model will be monitored through Key Performance Indicators. The Greater Huddersfield CCG info says that it has established new contractual, quality management and governance arrangements for this purpose. (Pre Consultation Business Case 48)
Let’s hope they’re better at this than Cambridgeshire and Peterborough CCG, who were unable to manage a huge 5 year “care of the elderly in the community” contract they awarded – after spending £1m on the procurement process, and after 8 months the contractor handed back the contract and walked away.
The Clinical Senate found it couldn’t figure out how risky the Care Closer to Home care model would be for:
- staff morale and motivation,
- worsening workforce issues,
- the quality and consistency of patient services,
- patient safety,
- the survival of GP practices and their valuable, trusted and much appreciated working culture,
- end of life care and geriatric services
- etc…
As a result, there is no telling if Care Closer to Home will provide the required standard of care.
(For more info, please see the section Lack of information about the Primary Care Strategy and how to ‘mitigate risks to patient care’, in Care Closer to Home part 3 – link coming soon.
Patients Self care
To cut the costs of caring for the frail elderly and people with chronic illnesses Phase 2 Care Closer to Home will also:
“strengthen supported self care”
(which seems to be basically getting family, friends and voluntary organisations to take care of patients), and develop a contact centre for stakeholders (who are these?) clinicians and patients (Pre Consultation Business Case, p44)
Greater Huddersfield CCG Care Closer to Home – Plans and Phase 2 – in section on Long term conditions – adults at risk of harm due to their frailty – says
“we believe that there is additional capacity to manage cases out of hospital, in addition there is the potential to deflect another 50% of people from the formal pathways of care”
What? Where are they going to be deflected to? Are they proposing that this extra 50% of frail adults will basically be told to sod off and look after themselves?
Greater Huddersfield CCG thinks that getting people to take on “self care” is their “big challenge”
This is according to a document I obtained through a Freedom of Information request.
This states that their big “challenge” in setting up Care Closer to Home is:
“Realigning the mindsets of individuals, their carers and their health professionals to this vision.”
It all sounds a bit like North Korea to me.
Why should the patients, carers and health workers who are going to be affected by Care Closer to Home need their “mindsets” “realigning” to its “vision”?
Particularly since the CCGs are at pains to say that Care Closer to Home is giving patients what they’ve told the CCGs they want.
I asked Greater Huddersfield Clinical Commissioning Group this question at their AGM in July 2015. Dr Judith Parker, the GP Practice Rep, told me:
“Realigning patients’ and their carers’ mindsets is about resilience and self management – a different way of health services – enabling and empowering people to take care of themselves and control of their health needs.”
But “resilience” and “enabling and empowering people” are code words for cutting public services, making patients and carers take the burden of care, and radically downgrading clinicians’ working practices, terms and conditions.