This is the 7th Plain Speaker report on the hospital cuts plans that are scheduled for public consultation, starting at the end of February.
It looks at proposals for expanding Calderdale Royal Hospital into a 615 bed acute and emergency hospital – the only one in Calderdale and Kirklees.
The “Right Care Right Time Right Place” Pre Consultation Business Case could well be called “Less Care, Whenever and Wherever You Can Find It”
The basic plan is to
- Knock down HRI, and sell off the site for development.
- Build a 119 bed planned care clinic plus outpatients and and urgent care centre on Acre Mill – leaving Kirklees without an A&E.
- Take services out of the hospital and put them in the community (so-called Care Closer to Home).
- Expand CRH from 400-ish beds to 615 and make it the unplanned (acute) care hospital and “emergency care centre” for both Kirklees and Calderdale, plus an urgent care centre
- Cut 755 staff and around 77 hospital beds,
- Set up an urgent care centre in Todmorden. (The urgent care centres would befor minor ailments and accidents. The independent clinical senate review worries that the urgent care centre staffing proposals are inadequate: they don’t guarantee a doctor would be present and they would rely on skyping colleagues in the Emergency Care Centre for advice) Update 5 March: The Clinical Commissioning Group has abandoned the proposal for a Tod urgent care centre.
- Take extra A&E patients to CRH, as a result of the closure of Dewsbury A&E and its replacement with an urgent care centre
In this report you can find out about:
- An A&E – but not as we know it
- What an “Emergency Care Centre” is
- Proposed acute and Emergency Department services at CRH
- The proposal to close the A&E in the area with the highest “disease burden”
- Increased death rates in hospitals with an A&E, when a nearby A&E closes
- Lack of evidence that halving the existing A&E service is going to be safe
- Lack of evidence that “new models of care” will cut “avoidable” emergency admissions
- Travel implications -plus more detail here
- Triage-only attendance at the “Emergency Care Centre”
- Intermediate care – one of the systems the CCG’s are relying on as an alternative to A&E – is a mechanism for restricting access to NHS care
- Links to the other Plain Speaker reports on different aspects of the hospital cuts plan
Please tell your MP to vote for the NHS Reinstatement Bill on 11 March 2016
The only real solution to the problems that the Clinical Commissioning Groups hope to solve through their hospital cuts proposals is to restore the NHS to a fully publicly owned, run and funded health service, that it is the duty of the Secretary of State to provide, and that restores its founding principles of universality, comprehensiveness and being free at the point of need. Please ask your MP to vote for the NHS Reinstatement Bill in the House of Commons on 11 March.
An A&E – But Not As We Know It
The proposed 615-bed acute and emergency Calderdale Royal Hospital – the only one in Calderdale and Kirklees – would provide acute/emergency medicine, A&E services in an “Emergency Care Centre” plus Paediatric Emergency Department, and an urgent care centre.
At the 20th Jan joint Clinical Commissioning Groups’ (CCGs’) Governing Bodies meeting to rubber stamp the decision to consult the public on the plan, a governing body member said:
“I’d like to clarify that this is a very different new model of urgent and emergency care than is currently in place.
There will be an urgent care centre in the planned care site and an urgent care centre in the unplanned care site, along with an emergency care centre that will function quite differently from A&E.”
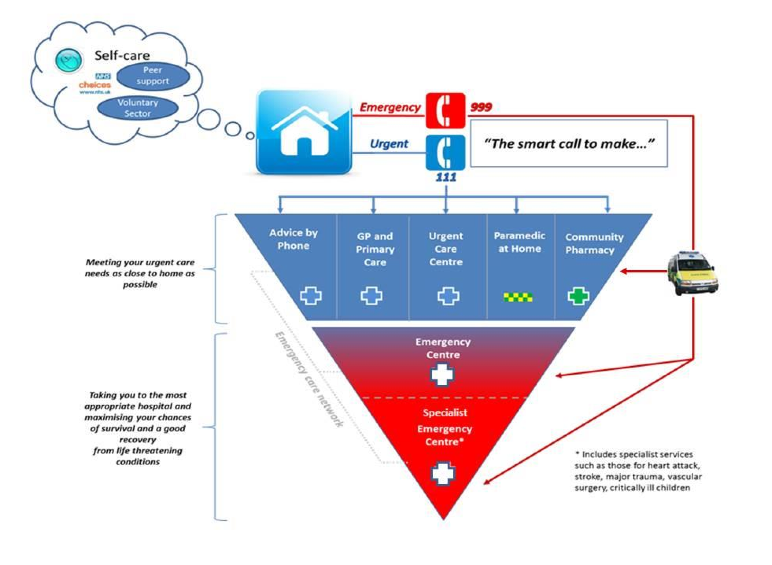
What is an Emergency Care Centre?
Not knowing what an Emergency Care Centre is, and with the CCGs refusing to say at their North Korea- style meeting on 20th Jan, I was fortunately put in touch with a friendly A&E consultant, who said:
“I’m unfamiliar with the term “Emergency Care Centre” as are those of my colleagues I have asked about it, in addition the Royal College of Emergency Medicine make no reference to it as a recognised entity. What I have found so far are centres bearing this name in Wigan, Gateshead and Cambridgeshire.
What they all share in common are the presence of an Emergency department (A&E) and an Acute or Medical Assessment Unit (AAU or MAU) with the variable inclusion of GP services, an Urgent Care Centre (UCC) or Walk In Centre, Urgent Children’s services and a Surgical Assessment Unit.I suspect that these are in fact what the Keogh Urgent and Emergency Care Review refers to as “Emergency Centres” in their Safer. Faster. Better document . If so then the CCG should be pressured into confirming that their Emergency Care Centre will have at its core an Emergency department; any other configuration would be something so far unknown and I suspect unlikely to receive the approval of the Royal College of Emergency Medicine.”
The Right Care Right Time Right Place (PCBC) says the Emergency Care Centre (ECC) planned for Calderdale Royal Hospital (CRH) would have at its core an Emergency Department, with a similar set of acute and A&E services as are in the current A&Es – but only on one site, instead of 2 on 2 sites that share some services across both sites.
The PCBC also says:
“The ECC would specialise in treating people with serious or life threatening emergency care needs, through Emergency/acute medicine and A&E services, with all the necessary acute facilities and expertise on the one site 24/7.”
From the PCBC, it does look as if the ECC planned for Halifax is, like the A&E consultant thought, an Emergency Centre – in the middle of Keogh’s 3 tier urgent and emergency care structure, as far as I can make out.
Presumably the Specialist Emergency Centre that the PCBC refers to is Leeds General Infirmary?
Calderdale and Huddersfield people are already taken there directly, following ambulance protocols, for:
- heart attacks meeting certain criteria
- major trauma
- complex vascular cases
- quite a few complex fractures such as those needing complex surgical procedures like Ilazarov frames
Commenting on facebook, a Yorkshire Ambulance Service paramedic said;
“We have been doing this for years and don’t have a choice. So when people mention we pick and choose which A&E we go to its untrue. We follow strict protocols or we get into trouble!”
Proposed acute and Emergency Department services at CRH
At the ECC, there would be a trained, experienced emergency medicine doctor and an A&E consultant 24/7, and “improved access to senior and specialist doctors on a rota.”
According to the PCBC, CRH would have a range of acute services that would integrate with the Emergency Department:
- acute medicine,
- acute elderly & frailty,
- Comprehensive Geriatric Assessment,
- respiratory care,
- stroke
- community hub (eg crisis intervention, RAID)
However at the Greater Huddersfield CCG Governing Body Meeting on 10 February, apparently the CCG said that stroke and heart attack patients will be transferred to Leeds. (If this scheme goes ahead.) So maybe they’re making it up as they go along?
The proposed Emergency Care Centre would have 8 unplanned operating theatres including :1 x 24 hour emergency theatre, 1 trauma theatre & 1 emergency obstetrics and gynaecology theatre.
It would include a Medical Assessment Unit.
Going into more detail, the PCBC (p55) says:
“…in the proposed model for emergency care, we would propose to co-locate the following services:
- Acute/general/elderly medicine
- respiratory (inlcuding bronchoscopy)
- Obs/gyn
- Neonatology (SCBU)/paediatrics (incl surgery)
- Upper and lower GI surgery (inc acute endoscopy)
- Trauma and orthopoedics
- Intensive Care Unit/24 hour anaesthetics
- Urology
- Gastroenterology
- ENT
- Acute Mental Health
- Cardiology (including CCU which I think is Coronary Care Unit)
- Hyper acute stroke services
- X-ray, USS (Is this Ultra Sound Scan?) MRI, CT, other diagnostics 24/7
- Microbiology/haematology/biochemistry
- Occupational Therapy
- Physiotherapy
They are proposing to close the A&E in the area with the highest “disease burden”
The Pre Consultation Business Case says that the biggest areas of deprivation are in and around Huddersfield, and it also says that along with high levels of poverty and deprivation in Huddersfield there is also “a higher disease burden”, with frailty, emotional welfare, obesity and cardio-vasular disease (CVD) as cause for specific concern locally.
The PCBC Equality Impact Assessment says (p 260) that the people most affected by putting all the Huddersfield and Calderdale A&E and acute services on one site are younger people, older people and disabled people, and that:
“There is a potential for a negative impact impact for those groups using Emergency Medicine or Acute services, if there will only be one centre, the majority of older people are living in rural areas (causing transport issues) and people with a disability may find access more difficult.”
Death rate increases in hospitals which still have their A&E when a nearby one closes
Dr Renee Y Hsia, the senior author of a 2014 study in the USA which found that the death rate increases in a population that still have their own A&E – but have to share it with newcomers who have suffered closure of their own A&E, said:
“Emergency department closures generally happen in vulnerable communities, but their ripple effects extend to other hospitals. While many people hearing about an emergency department closing at a hospital that is not where they normally would go may feel relief , it’s important for people to know that it still does affect them.”
Dr. Rebecca Parker, a member of the board of directors of the American College of Emergency Physicians, who was not involved in the study.
“An important part of the puzzle is which hospitals are closing down: they’re the ones located in underserved areas with poorer populations.”
The researchers in the 2014 study found that among inpatients at hospitals affected by an emergency room closure, 5% were more likely to die than patients at other hospitals. The increase in the risk of death for affected adults under 65 was even greater: their risk of dying in the hospital increased by 10% compared with similar patients who were not affected by a closure.
Heart attack, stroke and sepsis patients faced a 15% greater risk of dying in the hospital if there had been a closure nearby, when compared with similar patients at unaffected hospitals.
The study said emergency room closures at nearby facilities may contribute to mortality at other hospitals because they increase the distance and travel time to an emergency room, while exacerbating crowding and prolonging waiting times for care.
A&E closures may also cause some patients to postpone seeking care, so that they are in worse shape by the time they arrive at a hospital.
Where’s the evidence that halving the existing A&E service is going to be safe?
At the best, they’re cutting the existing A&E service in half, by putting everything in Halifax.
Updated 26 Feb – newly released travel analysis based on Dewsbury A&E closure Sept 2016
They plan to send Huddersfield patients to whichever is their closest A&E, not necessarily to Halifax. Given the geographical spread of Kirklees, that could mean they get sent to Barnsley or Pinderfields which are both hideously overcrowded.
The Pre-Consultation Business Case (p77) said that 85% of Calderdale and Kirklees A&E patients would go to CRH, which they say would mean 81,370 Yorkshire Ambulance Service journeys (patients)/year. But it turns out that this doesn’t include “modelling” based on the fact that Dewbsbury District Hospital A&E is to close come September 2016 when it downgrades to an urgent care centre.
The CCGs finally released their travel analysis a couple of days ago which includes modelling based on the closure of Dewsbury A&E.
This updated modelling shows that 91.9% of Calderdale & Kirklees A&E patients would go to Calderdale Royal Hospital A&E, which they say means 84,534 Yorkshire Ambulance Service journeys (patients) each year.
2% will go to Barnsley – 1,794 YAS journeys/patients. The CCGs’ travel analysis says this means an increase of 1,451 patients more than currently go to Barnsley A&E from Kirklees.
The CCG’s travel analysis doesn’t mention this, but Barnsley Hospital Foundation Trust records extreme risk status on a number of targets that relate to its ability to absorb an increase in attendance following the proposed closure of the A&E department at HRI.
- Emergency Department mid grade staff recruitment is RED.
- A&E 4 hour target is only 88% met and is RED.
- The Trust is in serious deficit showing RED on two counts.
These recorded risks are shown on P 41 of the February 2016 Trust Board papers within the Corporate Risk Report. This document is downloadable here.
And while they’re busy planning an extra 293 A&E patients/year from Kirklees to Pinderfields – where 586 ambulances/ A&E patients had to wait 60 minutes or more for handover into A&E during the year Dec 2014- Dec 2015, the downgrade of Dewsbury A&E to an urgent care centre in September 2016 will increase Emergency Department activity in CRH by an estimate 7 ED attendances/week.
Despite this, the PBCB justifies this more-or-less halving of the current A&E service for Calderdale and Huddersfield by saying (p54) that because of the “new models of care”, there would be a “smaller number of patients with Emergency Care needs”.
The PCBC is relying on these “new models of care” to reduce unplanned medical hospital admissions by 6%/year (p83) which would mean “ Significant delivery of commissioner QIPP” (ie save the CCGs quite a lot of money).
On p 89, the PCBC says that estimates of emergency attendances are based on “modelling”; the problem is, modelling is only as good as the assumptions it’s based on. What assumptions was this modelling based on? The CCGs need to tell us.
The example of modelling for PFI hospitals show how easy it is to fiddle this to get the answers you want on paper, which turn out to be impossible in the real world.
These claims, like all the other PCBC claims about quality and standards, need to be read against the Clinical Senate’s statement that both the hospital services and community services proposals are so unclear that they can’t:
“answer questions regarding the ability of this model to deliver the standards proposed.”
As well as hoping for reduced numbers of patients attending A&E – or the “Emergency Care Centre” – they are planning to push patients through faster, once they’re admitted to the acute hospital.
The length of stay in hospital would reduce eg
- medical admissions, 6% length of stay reduction,
- paediatrics 10% reduction in length of stay, 5%
- maternity 5% reduction in length of stay etc.
All Trauma and orthopoedics, general surgery and urology inpatients with a length of stay of more than 10 days would be shifted to Huddersfield if clinically appropriate.
The imminent downgrade of Dewsbury A&E to an urgent care centre will increase ED activity in CRH by an estimate 7 ED attendances/week.
Evidence is lacking that “new models of care” will cut “avoidable” emergency admissions
Evidence is lacking that the “new models of care” – based on moving services out of the hospital – will reduce so-called avoidable emergency admissions, and so make it safe to cut 77 hospital beds, 755 hospital staff and one A&E by 2020.
A Nuffield Trust briefing (NHS hospitals under pressure: trends in acute activity up to 2022) said that plans to replace acute and emergency hospital services by care in the community are not likely to work, given the evidence that:
“To date, attempts to reduce the numbers of people admitted to hospital through better preventative care in their communities have not been very successful on a large scale” ( p2)
“Current policy is aimed at cutting the number of emergency admissions by providing more, better services outside hospital that can either prevent the need for hospital admission or offer the same care but in different settings. This is a common theme in initiatives for more integrated services, including the government’s Better Care Fund. But there is little evidence that this can be achieved.(Bardsley and others, 2013).” (p11)
A 2014 review of the evidence for promoting “integrated care” out of hospital found that:
“a close look at the data highlights a dearth of evidence on the impact of integrated care”.
Reporting on its Commission on Hospital Care for Frail Older People, the Health Service Journal (November 2014) stated
“There is a myth that providing more and better care for frail older people in the community, increasing integration between health and social care services and pooling health and social care budgets will lead to significant, cashable financial savings in the acute hospital sector and across health economies. The commission found no evidence that these assumptions are true.”
Social care has been plagued for decades by cuts, outsourcing and piecemeal privatisation of services, leaving many staff on zero hour contracts and service users with 15 minutes sessions of care. There are very real fears that the integration of health and social care will mean the plundering of already inadequate NHS budgets to prop up local government services.
The danger is that under local authority rules integrated health and social care will mean that there will be means-tested charges for services rather than the NHS principle of services funded from general taxation.
The outcome may be a deregulated, local service – partly privatised, its social care component already 90% privatised – facing a meltdown in local authority finance, competing with other localities for patients and funds, with local pay and conditions for health workers, and all branded as “integrated”.
Increased pressure on Yorkshire Ambulance Service and increased travel times
Closing Huddersfield A&E would mean 10,071.86 hours extra Yorkshire Ambulance Service journey time/year. If Halifax A&E were to close and Calderdale patients were sent to Huddersfield A&E, this would mean an extra 8,787.17 hours extra YAS journey time/year.
Given that YAS is currently struggling to cope with what it already has to do, how is it going to cope with an extra 193 hours more journey time/week if Huddersfield A&E were to close?
The CCGs’ travel analysis report says:
“It is recommended that the RCRTRP Programme Board and YAS examine the findings of this report and agree the implications on the options for the wider reconfiguration of hospital services across the CHFT/Calderdale and Greater Huddersfield CCG areas.”
So, what does YAS make of having an extra 10,072 hours/year journey time if Huddersfield A&E closes?
And what of the effect on patient mortality of “average” increase of 6.48 minutes for ambulance journey times? Which if you factor in the effect that half of journey times will be unchanged (the ones for Calderdale A&E patients) this means that the “average” increase in ambulance journey time for Kirklees patients will be double that, ie 13 minutes more in the ambulance.
Triage-only attendance at the “Emergency Care Centre”
One thing is clear from the Pre Consultation Business Case (p165): the proposed Calderdale “Emergency Care Centre” would only take patients who’ve been sent there “through some sort of clinical triage. “
None of us from either Calderdale or Kirklees would be able to just pitch up there like we can at the moment.
Instead, you would be triaged at the nearest urgent care centre in Huddersfield, Halifax and Todmorden, or via your GP or walk in centre, or a YAS paramedic, and then sent to the nearest A&E – not necessarily to Halifax, according to what the Preconsultation Business Case says.
It also says that patients would be able to get acute medicine services without admission to hospital. This would be through rapid-access outpatient clinics, ambulatory, rapid response community alternatives (what are these) or intermediate care.
Intermediate care: a mechanism for restricting access to NHS care
I had to look up “intermediate care”. It turns out it is a concept introduced by the New Labour government in its 2000 NHS Plan for England, which continued the market oriented and pro-business NHS policies begun under previous Conservative governments.
A 2004 British Medical Journal article states :
“… little scientific evidence exists on the benefits of intermediate care… The term intermediate care is often used as if its meaning is clear, but it conveys little meaning other than being about care that is “in between.”…The concept seems to arise out of a policy imperative, rather than an analysis of the scientific evidence about effective models of care.”
It seems that the policy imperative was to use the New Labour 2000 ‘concordat’ with the private sector to bring private hospitals and nursing homes into the mainstream of NHS service provision. The Concordat included providing intermediate care in nursing homes and the community, as one of the ways in which the private sector would become
“a permanent feature of the new NHS landscape.”
In NHS plc (31) Professor Allyson Pollock says
“…the Labour government not only endorsed the Conservatives’ removal of long-term care from the NHS, but has also used the resulting blurred boundary between health care and ‘personal care’ to start curtailing people’s rights to other kinds of health care by reclassifying it as “intermediate” care.”
By time-limiting NHS care for the first time in its history, it ended the inviolable NHS principle of care that is free at the point of need. Intermediate care – most likely provided by a private nursing home or in the community – is free at the point of need for the first 6 weeks but after that it becomes a joint NHS and Council responsibility and patients may be – and almost always are – charged for it on a means tested basis.
So now we know what intermediate care is a means to deny patients NHS care, to enable private companies to profit from providing long term care, and to charge patients for needing it.
Staffing
The PCBC says that putting all the A&E in one place will make if possible to provide the recommended minimum of 10 A&E consultants per emergency department. (p 69)
But on p98, referring to the problems the hospital Trust has with finding and keeping enough A&E consultants and acute paediatricians, the PCBC says:
“…recruitment difficulties reflect both national shortages of emergency doctors (nearly one fifth of consultant posts in ED department are either vacant and filled by locums) and local factors, such as the lack of ED subspecialisation (eg paediatrics and trauma)…”
But if trauma is going to Leeds, that won’t help will it? Another question for the CCGs to answer.
Here are links to some more Plain Speaker reports on the Pre Consultation Business Case proposals:
- Two Towns One Fight – We need both A&Es
- “Care Closer to Home” – Patients Will Suffer
- Care Closer to Home – Too bad there’s little or no evidence it will work
- Impartial doctors can’t tell if unclear plan for Huddersfield hospital cuts & changes
- will provide required standard of care
- Wakefield and Dewsbury Hospitals Groaning Under “Clinical Model” Now Proposed for Calderdale & Kirklees
- A single “Emergency Care Centre” for both Calderdale and Kirklees – Not Safe, Not Fair
Superb analysis-I worked as a lay reviewer for CHI during the period that Blair’s New vision for the NHS was being touted/implemented, PFI ‘s etc and thought then it was a huge mistake, but I didn’t realise the real agenda was privatisation by stealth!
Thanks Nancy, if you’re on fb or twitter, please will you share this post as widely as possible? People need to know! You must have had an interesting time as lay reviewer for CHI.