Last year saw big protests against proposals to close Calderdale A&E and other acute Calderdale Royal Hospital services like acute paediatrics and complex maternity, and to transfer hospital services for the frail elderly and people with chronic illnesses into GP-run services in four “localities” in Calderdale, in the hope that this will reduce acute and emergency admissions.
Although there is no evidence that this will work, these so-called “Right Care Right Time Right Place” and “Care Closer to Home” plans haven’t gone away – far from it.
Dr Matt Walsh, Chief Officer of Calderdale Clinical Commissioning Group (CCG), told the 11th June CCG Governing Body meeting that these plans are now accelerating, as a result of the Tory government’s pressure since the election. He said,
“Work is going on apace on future models of service delivery.”
These “future models” are about to be tested in the Upper Valley, in a so-called “Vanguard Multi-speciality Community Provider (MCP) Scheme” that is due to be in place by June 2016.
Calderdale is one of 29 areas in England that are part of the new “Vanguard” scheme, funded by NHS England to test “new models of care” that are more “sustainable” and “affordable”.
The aim is that the new models of care will cut costs in line with the £22bn /year NHS funding shortfall that is projected for 2020.
GPs’ new private shareholder company to take leadership in Vanguard scheme
Although the CCG Governing Body meeting didn’t mention this, 23 of Calderdale’s 25 GP practices have set up a private shareholder company called Wainhouse Healthcare Ltd, aka Pennine GP Alliance, in order to put GPs in a clear leadership position in redesigning the NHS, as the GP Alliance’s CEO John Tacchi told Plain Speaker.
Aiming to deal with the shortage of GPs and the stress and pressure on GPs because of increasing demands on them, Wainhouse Healthcare Ltd/Pennine GP Alliance has been involved in the Calderdale Multi-speciality community provider (MCP) Vanguard scheme from the start.
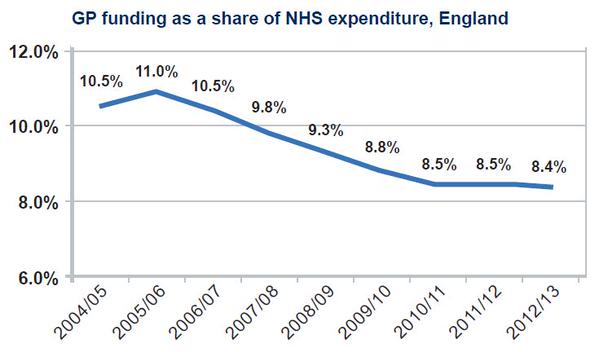
Critics of such GP Federations say that their formation has been engineered by government cuts to GP funding, that are designed to lead to commercialised/privatised primary care. The British Medical Association – the GPs Trade Union – is urging people to write to their MPs to call for restoration of proper funding for GPs and other measures to safeguard the future of the NHS.
A former merchant banker who recently graduated from the NHS Fast Track Leadership Programme – a new 10 month scheme to turn 50 hospital consultants, GPs and people with business experience into senior NHS executives, Wainhouse Healthcare Ltd’s CEO John Tacchi said,
“The old style of the single practitioner GP practice, based on the GMS contract, is dead. Pennine GP Alliance wants the flexibility to allow GPs to work together in a bigger unit legally.
Because GPs run their own business, they’re used to making commercial decisions. So someone with commercial experience might be valuable to Pennine GP Alliance, together with my history of running SMEs and advising SMEs.”
Update: Calderdale Local Medical Committee recorded members‘
“overwhelming support… for formal collaboration”
Perceived advantages were all about money and gaining contracts:
- “Practices become the navigators and coordinators of care for patients; controlling the effective use of resources for current services and work collaboratively to develop new community-based ones
- “Better use of resources; cost sharing agreements; increased access to wider patient populations thereby increasing income and improving profitability
- Collective strength, being attractive to commissioners through having access to larger cohorts of patients and a larger geographical area.”
Dr Alan Brook, the Chair of Calderdale Clinical Commissioning Group Governing Body, whose Longroyde surgery is a member of Wainhouse Healthcare Ltd/Pennine GP Alliance, described the Calderdale Multi-speciality Community Provider Vanguard scheme as:
“an innovative test for Right Care Right Time Right Place.”
He said:
“There are increased risks in the health care system because existing care models are not sustainable or affordable – we need to change them quicker to reduce these risks.”
However, the Calderdale CCG risk log presented to the CCG Governing Body shows a serious risk (level 16) that the proposed new Right Care Right Time Right Place model will not work – resulting in poor services, lack of financial benefits from new system and inability to change hospital and community services in ways needed to deal with quality, finance and workforce issues in the CCG’s case for change; this includes the need to help fill a £154.5m funding gap over the next 5 years.
Contract dispute between the Calderdale and Huddersfield hospital trust and the CCGs
Since the election, the drive for NHS cost cutting has increased, as it’s become clear that the government will not provide any extra money this year, despite the fact that 149 hospitals (including Calderdale & Huddersfield hospitals trust) are already in deficit.
Our hospitals Trust is forecasting a £20m deficit, assuming that it can make £14m “efficiency” cuts.
Far from providing extra money, the government has just cut £200m from the public health budget – while trumpeting the importance of preventive health care (which is what public health services are all about).
Calderdale Clinical Commissioning Group’s Chief Finance Officer Julie Lawreniuk told the 11 June CCG Governing Body meeting that the CCG’s money is getting tighter in 2015-16 as the available pot of money is shrinking.
The CCG’s 2015-16 contract with the hospitals Trust has not been signed and the Trust has referred both Greater Huddersfield and Calderdale CCGs into a dispute resolution process. The Trust is looking for £10m extra across both CCGs and has also opted for a “payments by results” contract rather than the block contract it has had before.
NHS England has noted in a letter to Dr Walsh that payment by results:
“is very risky for the Trust. The CCG have tried to persuade CHFT that what they are offering is a good deal but they are not in agreement.”
Ms Lawreniuk told the Governing Body meeting that payment by results was like putting a bar code on the head of each patient and swiping it for each treatment they received. GP Dr Caroline Taylor said this can affect the new Care Closer to Home models of working – it could make it difficult to pay GPs and other community health staff.
Dispute with hospital over contract won’t stop CCG from going ahead with “new model of care” in the community
Dr Walsh said,
“This isn’t going to get in the way of the CCG delivering Care Closer to Home, but it makes it more difficult to work in partnership with CHFT” [the hospitals Trust].
Dr Walsh told the CCG Governing Body meeting that NHS England’s Vanguard scheme gives Calderdale the chance to bid for a share of £200m to set up a “new model of care”, and that the Calderdale “local health economy consortium” is “having a conversation about clarity for its bid”.
He said that the Calderdale Vanguard scheme in the Upper Calder Valley will:
- Start by demonstrating the potential for providing frail elderly people with health and social care in a GP setting and at home, so that they are less likely to have to go into hospital for unplanned/emergency care.
- Then apply learning from that to people with long term illnesses, children with complex care needs and people who need urgent care.
I asked the CCG Governing Body how they could go ahead with the Vanguard scheme when they still haven’t consulted the public on the Right Care Right Time Right Place “transformation” of Calderdale NHS and social care that the Vanguard scheme is supposed to test.
Dr Brook said,
“It’s entirely possible to go ahead with the Vanguard scheme, but the content of the proposed public consultation is not finalised…Our plans are to provide hospital services that are sustainable and fit for purpose. We don’t have clarity on how this will pan out.”
But Dr Walsh told the CCG Governing Body meeting that,
“The CCG is clear about the need to identify how to use Calderdale Royal Hospital to deliver value for the Private Finance Initiative investment, since the PFI charge for CRH is not going to go away.”
Dr Walsh said that there were some differences between the CCG’s doctors and hospital doctors over this issue.
Detailed exploration of case for Calderdale Royal Hospital as 85 bed planned care hospital with “additional commercial activities” worth £15m/year
On 16th April, Calderdale and Greater Huddersfield CCGs met with the hospitals Trust to explore in detail the hospital Trust’s Planned Care model, as presented last autumn in their Outline Business Case (OBC).
The Trust’s OBC proposes to make Calderdale Royal Hospital a small planned care hospital, carrying out planned treatments like hip or knee operations, with only 85 of its current 350 beds in use and no A&E, just a Minor Injuries Unit that would see around 22,500 patients a year.
The OBC sees a possible future for the “redundant” space in the rest of CRH as a care home and hospice, and says
“There is potential to link up with other Care Home or Hospice providers” (p141)
And this “spare capacity” at CRH could generate an extra £15m income from “additional commercial activities” (p175)
The Trust’s OBC proposes that 24/7 acute and emergency care would be at Huddersfield Royal Infirmary. This would include trauma, major surgery, critical care, acute & specialist medicine, inpatient paediatric services and complex maternity services.
In addition to minor injuries units, the OBC says both hospitals would provide outpatient care for children and adults, midwifery-led maternity units and specialist psychiatric liaison services.
“Major workforce challenges” ahead as hospital doctors and GPs disagree about how to provide out-of-hospital urgent care
The 16th April meeting between the CCGs and the hospital Trust also discussed the CCGs’ “potential model” for Urgent and Emergency Care.
Dr Walsh said that there were differences between the CCG doctors and the hospital doctors, particularly about urgent care models that allow “Care Closer To Home” and reduce the demand and burden on emergency specialists.
The issues were how to make better use of community urgent care services.
Dr M. Azeb, Calderdale CCG’s clinical lead on urgent care, asked about the issue of limited numbers of doctors and nurses to service the new community urgent care model.
Dr Walsh said,
“The CCG is expecting people to be more flexible and will put infrastructure in place for this. There are major workforce challenges in this transformation process.”
(NHS England’s Five Year Forward View wants a new “modern workforce” for the new care models. Features of this “modern workforce” are local pay, 24/7 working, flexible and able to “cross boundaries”, increased productivity and a reduced skill mix, changed terms and conditions and a huge new role for volunteers.)
Dr Brook added,
“There is a shortage of generalists. General Practice is the biggest workforce challenge facing the NHS. GPs can’t be the sole staff at community urgent care centres. The hospital is reluctant to staff community urgent care centres, but they’ll have to. These issues will go in the pre-consultation business case.”
Will the “multi-speciality community provider” end up running Calderdale Royal Hospital?
Wainhouse Healthcare Ltd’s CEO John Tacchi told Plain Speaker,
“Pennine GP Alliance is saying that the MCP Vanguard has to apply to Calderdale as a whole – not just the Upper Valley. You can’t fix CHFT in isolation, you have to tackle whole health economy.
There’s no hard and fast view of what an MCP care model can be – it can blend into the Primary and Acute model.”
This Primary and Acute (PAC) model joins up GP, hospital, community and mental health services.
Its overlap with the Multi-speciality Community Provider (MCP) model is confirmed by NHS England’s statement that a “mature” MCP could take over the running of their District General Hospital (eg Calderdale Royal Hospital), as an Accountable Care Organisation.
American private health insurance company model
Also known as Health Maintenance Organisations, Accountable Care Organisations are accountable for providing care – but they do not themselves provide health care.
They originated in the USA as private health insurance companies like Kaiser Permanente and United Health – the previous employer of NHS England boss Simon Stevens.
Both Labour and Tory Parties support NHS England’s 5 Year Forward View and its plan of setting up Accountable Care Providers. Labour’s 10 Year NHS Plan explicitly endorses this and Tory Health Secretary Jeremy Hunt told Parliament before the General Election that clinical commissioning groups should become accountable care organisations.
Greater Huddersfield CCG has moved towards this Accountable Care Organisation model by awarding its £238m Care Closer to Home contract to a “lead provider” – although a month has gone by since it decided who to award the contract to and it has been unable to announce who this “lead provider” is. It is believed this is because the losing bidder is appealing against the CCG’s decision.
A “lead provider” is awarded a big contract and then subcontracts it. The subcontracts can go to a mix of NHS organisations, private companies and voluntary sector organisations. This can lead to problems of lack of accountability and fragmentation of care.
Asked if the Calderdale MCP care model is going to be contracted to Wainhouse Healthcare Ltd as the lead provider, John Tacchi said:
“I think it would be good idea and something we believe, but I can’t tell if it will happen. This will be clear soon.”
I asked how conflicts of interest would be avoided if Calderdale Clinical Commissioning Group were to award its own GP members in Wainhouse Healthcare Ltd the contract to run the Vanguard MCP scheme.
This has already been an issue in Kirklees, with the North Kirklees GP Federation Curo Health Ltd gaining a £0.5m contract from N. Kirklees CCG for a Care Closer to Home pilot.
John Tacchi said,
“This is a national issue – this is the weakness of commissioning but we’re stuck with what we’re stuck with now.
I’m not saying there is a conflict of interest, but without assurances to the public you’d be forgiven for assuming that there will be a conflict of interest.”
He continued,
“The result of the last reorganisation was fragmentation, with social care commissioned by the Council and Health care by the NHS.
What is needed is joint commissioning.”
As a Multi-speciality Community Provider, Wainhouse Healthcare Ltd could take control of the pooled health and social care budget that would exist under a process of joint commissioning by the Council and the Clinical Commissioning Group – although obviously none of these arrangements have yet been sorted out.
Under the new Tory government, there is now a particular need to accelerate joint commissioning, Dr Walsh told the 11 June CCG Governing Body.
He said that there would be a joint meeting the following week to discuss the recent Kings Fund document on integrated commissioning.
He added that DevoManc
“is a paragon of how to frame ambitions” for joint commissioning.
Dismantling the NHS and setting up regional health services
DevoManc is the devolution of the entire Greater Manchester £6bn/year NHS and social care budget, from the Treasury to a new Greater Manchester Strategic Health and Social care Partnership Board.
DevoManc was sprung upon Manchester through a secret deal between George Osborne and Manchester Council leaders Sir Howard Bernstein and Sir Richard Leese.
Its purpose is to drive through the Greater Manchester Healthier Together Programme, which plans to close 4-5 acute District General Hospitals in Greater Manchester and divert the funding into new “models of care” outlined in NHS England’s Five Year Forward View.
DevoManc has met with sustained opposition from the Greater Manchester Association of Trades Union Councils.
Although the scheme is called “Devolution of health and social care”, in fact NHS England has control of the £6bn/year Greater Manchester NHS and social care budget.
It will enforce its own models of care and “modern workforce”, through a Programme Board that supervises the lower joint commissioning boards. These are the GM Strategic Health and Social Care Partnership Board, and below that, Joint Commissioning Boards of local Councils and CCGs. NHS England has membership of each of these Boards.
The supervising Programme Board consists of:
- Simon Stevens (the head of NHS England and former head of United Health, the global American private health insurance company),
- John Rouse from the Department of Health,
- leading figures in the Greater Manchester Healthier Together programme
- Graham Unwin, Staffordshire and Shropshire Area Team Director – who brings experience of the contentious downgrading of Mid-Staffs hospital (which recently lost its A&E, paediatrics and maternity services), and of competitive tendering of the £1.2bn contracts for Transforming Cancer and End-of-Life Care Services for the Staffordshire area.
Dr Walsh said that Calderdale has a lot to learn from DevoManc and a long way to go.
He said the West Yorkshire Healthy Futures programme for cancer services, paediatrics, stroke services and urgent and emergency care is the precursor to these joint commissioning conversations, that are due to take place shortly.
999 Call for the NHS
As the government accelerates the pace of NHS cuts and sell offs, and the effects are felt in Calderdale, it’s time to make a 999 Call for the NHS.

Yes we already have this in Cramlington ,Northumberland and it is happening across UK, fight with all your might we managed to save some services ,NHS England call it centralisation,when they really mean downgrading services
https://www.facebook.com/groups/806306722748618/