The hospitals Trust has finally made public their Outline Business Case (OBC) for the shake up of hospital and community NHS services in Calderdale and Greater Huddersfield.
The OBC comes down on the side of making Calderdale Royal Hospital the small planned care hospital, carrying out planned treatments like hip or knee operations, with only 85 of its current 350 beds in use and no A&E, just a Minor Injuries Unit that would see around 22,500 patients a year.
24/7 acute and emergency care would be at Huddersfield Royal Infirmary. This would include trauma, major surgery, crticial care, acute & specialist medicine, inpatient paediatric services and complex maternity services.
In addition to minor injuries units, the OBC says both hospitals would provide outpatient care for children and adults, midwifery-led maternity units and specialist psychiatric liaison services.
The OBC sees a possible future for the “redundant” space in the rest of CRH as a care home and hospice, and says
“There is potential to link up with other Care Home or Hospice providers” (p141)
And this “spare capacity” at CRH could generate an extra £15m income from “additional commercial activities” (p175) – I guess, from the use of CRH by other care home or hospice providers.
The OBC develops the economic, commercial and financial case for proposals made in the spring in the Strategic Outline Case (SOC):
- cutting acute and emergency hospital services,
- splitting hospital services between a small planned (elective) care hospital and a bigger acute and emergency hospital,
- increasing care in the community to make up for the cut hospital services.
In April 2014, Calderdale Council rejected the SOC as unfit for the people of Calderdale and asked the hospitals Trust to withdraw it.
Calderdale Clinical Commissioning Group considered the OBC on October 27th, but hasn’t yet said what it thinks of it, as far as I know.
The OBC recommends that both Calderdale and Greater Huddersfield CCGs consider the OBC and start formal public consultation on options 2 (HRI as the acute and emergency (unplanned care) hospital and 3 (CRH as the acute and emergency (unplanned care) hospital.
It says the 3 providers would be happy to consider Option 5 – new proposals that emerged during the public consultation. This sounds like the best bet to me. So people, let’s get our thinking caps on.
It acknowledges that the commissioners may have other ideas of their own that they’d rather consult the public on. No doubt we shall eventually find out about this.
Recommendations made on the basis of unsupported assumptions
The OBC says its recommendations are evidence-based and based on “detailed modelling”.
As an example, it says that despite inevitable rises in demand for hospital services due to population growth and growing numbers of old people, it will be possible to get away with cutting acute and emergency hospital services by introducing new ways of working and increasing community health services – particularly for frail older people and people with long term illnesses.
This flies in the face of the recent National Audit Officer report that found,
“limited evidence that integrated care is cost-effective in sustainably reducing hospital admissions.”
It also flies in the face of findings from the recent Health Service Journal Commission on Hospital Care for Frail Older People. This blasts NHS England’s latest “Messiah concept”: that providing more integrated care closer to home for frail older people will solve the problem of poor care or lead to a sustained, long term reduction in hospital admissions.
The HSJ Commission’s Report calls this a “myth” and an example of “magical thinking”, while pointing to a history of failed NHS Messiah concepts – such as lean, Toyota, community matrons and case management pyramids.
The OBC’s evidence and modelling may be shakier than it should be. When you read on past the figures for forecast reductions in “hospital bed based activity” -ooer Matron – you find that these reductions are based on a number of assumptions.
One assumption is that the increased provision of community care will cause a 40% reduction in admissions to Geriatric Medicine and a 15% reduction in admissions to Neurology, Respiratory Medicine, Stroke Medicine, Cardiology and a bunch of other ologies.
But what are these assumptions founded on? Nothing about that in the OBC.
“Before long the frail elderly will be wandering the streets like a zombie apocalypse”
The HSJ Commission’s Report quotes Professor Marion McMurdo, Professor and Head of Ageing and Health at the University of Dundee and a consultant geriatrician, as saying:
“The acute care of older people has progressed from being an inconvenience to being an anathema.”
And it endorses her “radical suggestion” that we should “make hospitals good places for old people” – instead of making the ageist inference that hospitals’ “core business” of caring for old people is too tricky to manage and the problem can best be solved by ceasing to attempt to deal with it.
Without this, Dr Jonathan Tomlinson has tweeted that,
“Before long the frail, elderly with nowhere to go will be wandering the streets like a zombie apocalypse.”
Is this the future for our old people in Calderdale?
A&E – NHS England’s latest update on dealing with A&E pressures abandons idea of cutting and centralising A&E departments
In terms of A&E – a key issue for us in Calderdale, who stand to lose our A&E under the recommendations in the OBC – there is a projected reduction of 3% in A&E admissions over the ten years to 2023/4.
However, the evidence that this is possible doesn’t really exist, as has been made clear in discussions about the Better Care Fund, which transfers money from the Trust to the Councils, in order to fund more community health and social care with the aim of keeping people out of hospital and cutting A&E admissions.
Actual predicted numbers of A&E admissions are that by 2023/4 there will be 22,563 admissions/year to the Minor Injuries Unit at CRH, 117,364 admissions to A&E at HRI and just over 3,000 admissions to Minor Injuries Units in Tod and Holme Valley.
The OBC says that there would be “no significant impact” on ambulance services, because
“All areas are still within a 45 minute travel time.”
Which a lot of local people with knowledge of the roads and traffic would contest.
The reasons for closing CRH A&E and sending all A&E patients to Huddersfield were given in the 2013 National Clinical Advisory Team Report, and were based on the recommendations of the Keogh Review that proposed cutting the number of A&E departments across the country from around 140 to between 40-70 “major emergency centres”.
But in August 2014, NHS England’s Update on Keogh’s Urgent and Emergency Care Review has dropped these proposals. It acknowledges the pressures on A&E that Keogh identified need dealing with, but says “the challenging issue” is how to deal with them.
The way this Update rows back from proposals to cut the number of A&E departments has to raise questions about the validity of the OBC proposals to close Calderdale A&E.
The Tod and Holme Valley Minor Injuries Units would be staffed by Emergency Nurse Practitioners and would only treat adults. Children would have to go to the Paediatric A&E in Huddersfield – or to the Minor Injuries Unit at CRH, if their health problems were minor eg didn’t involve breathing difficulties, allergies, any problems usually dealt with by a GP, major injuries, loss of consciousness, mental health problems etc.
The OBC jauntily says that, as far as travel times to A&E are concerned, people in the NW of Calderdale may go to a closer hospital than Huddersfield Royal Infirmary – but who knows where that might be?
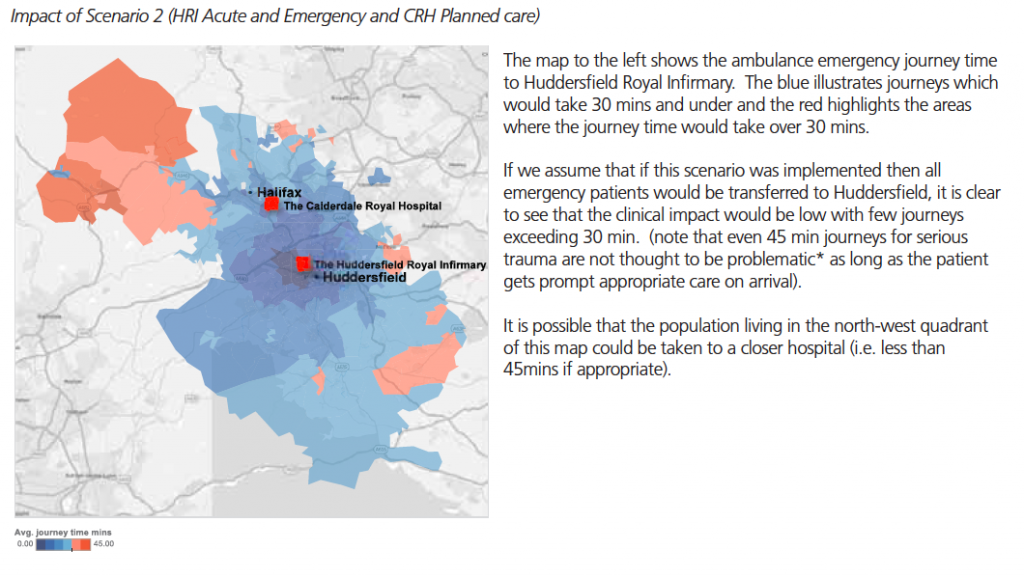
And the OBC’s predicted travel times to HRI A&E seem a bit optimistic to me.
Cuts to acute hospital beds
In terms of bed numbers, the OBC seems out of date – since it was written, the hospitals Trust has announced that because of a need to make £20m “efficiency savings” this financial year and £19m next financial year, it has to cut 110 beds between October 2014 and the end of March 2016.
Calderdale Clinical Commissioning Group has approved this 110 bed cut, which is in addition to the 299 bed cuts that the OBC plans to make by 2023/24.
112 of the OBC’s bed cuts represent a transfer of workload from acute hospital care to the community. (p 180)
According to the OBC’s modellng, it costs £60-65/day for an acute bed in the community, that avoids a hospital admission or accelerates hospital discharge. This compares to £300/day for an acute bed in hospital.
The OBC says that this is
“proof of concept that care closer to home is cheaper than acute inpatient care.”
But it notes that there are other costs associated with community care that need to be taken into account. It says that national evidence is that the real saving is about 30% compared to the 80% suggested by a bald comparison of the daily costs of an acute bed in the community and an acute hospital inpatient bed.
“Sustainability” of Calderdale and Greater Huddersfield NHS system is an issue, due to Trust’s deficit
Because of the need to make whacking great efficiency savings this financial year and next, in April 2014 the Trust was forced to produce its so-called Balanced Plan, to show how it could cut spending or raise income in order to save £20m this financial year and £19m next financial year – which it has so far been unable to come anywhere near doing.
The result is the Trust is now in deficit and receiving the unwelcome attentions of Monitor, the NHS privatisation quango which is urging the Trust to make harder and faster cuts.
Because of the hospital Trust’s deficit, which has become an issue since the OBC was written in the early summer, it’s no longer clear that, on its own terms, the Trust is in a position to make the changes proposed in the OBC.
The OBC says,
“All models proposed within this outline business case are predicated upon maintaining a Continuity of Service Risk Rating of 3 in each year.”
The Continuity of Service Risk Rating is a key measure of sustainability not only for the Trust, but for the whole Calderdale and Greater Huddersfield NHS system. Sustainability as in, whether there’s enough money to keep it going.
3 is a good measure. 4 is the best.
But because of the Trust’s deficit, Monitor, the NHS privatisation quango, has increased its Continuity of Service Risk Rating to 2.
Level 1 indicates significant risk.
Even before the Trust was in deficit and its sustainability became more at risk, the OBC estimated (p178) that the Trust would lose £19m income over the 10 year period due to transferring services from the hospital to the community, but could only see cost savings of £14m, meaning that somewhere £4m efficiency cuts would be necessary.
More later – the NHS funding shortage, workforce cuts and timing of public consultation and implementation.
The OBC is frank about the NHS funding shortage that is driving these proposed changes.
There is a lot more in the OBC about funding, workforce cuts and the proposed timeframe for consultation and implementation. I will return to this in a later report.
Reasons for delay in publishing the OBC
The Trust had previously refused to publish the OBC on the grounds that it was commercially confidential.
This is because it was produced by the Trust, working together with Locala, the Kirklees community health company, and with the mental health Trust. It contains information that both Locala and the mental health Trust used in their bids for the £284m Care Closer To Home contract that GH and NK CCGs put out to tender.
Now the deadline has passed for submitting bids for that contract, the OBC is no longer commercially confidential.
The OBC is online here.
Updated 30/11/2014 with info about NHS England’s August 2014 Update on Urgent and Emergency Care Review


Pingback: Save Calderdale Royal Hospital | Calder Valley Greens - Jenny4MP
Jenny Could you let me know where I can read the full business plan. In my own time is it on the ,trust,s web site ? Regards Barrie Boon.
I’ve added the link to the OBC (which I’ve uploaded to the Scribd website) right at the end of both Plain Speaker posts about the Outline Business Case. Hope you can find it ok. If not please let me know and I’ll email it to you.
And why did the Trust had previously refused to publish the OBC on the grounds that it was commercially confidential yet Locala could see and help prepare their bid? Is that not giving Locala an unfair advantage? Of coarse it is. This whole process is corrupt, has nothing to do with care and all to do with political doctrine hence no public consultation.
Thanks Jenny for this analysis. All of us who are “served” by CHFT should see how they care about our future services. They should be shouting from the rooftops about the lies coming from the Govt and the DOH about ringfencing spending on the NHS.