As expected, both Calderdale and Greater Huddersfield NHS commissioners today agreed to postpone the public consultation on proposed hospital cuts and changes. The consultation had been scheduled to start this month.
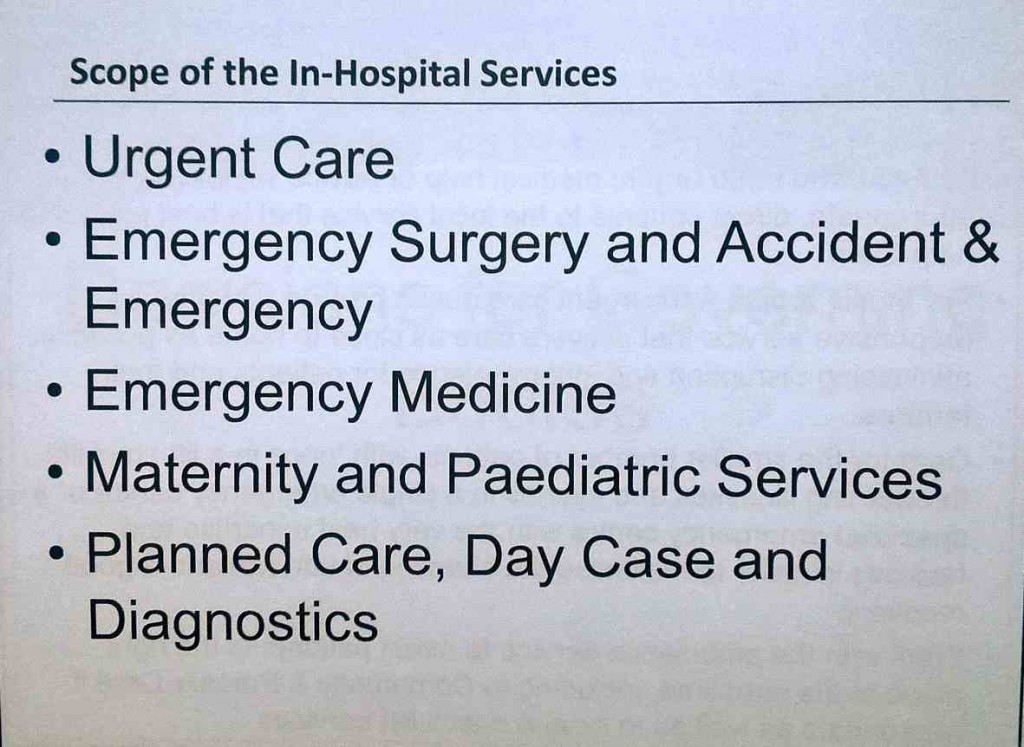
One burning issue for the public is what NHS bosses want to do to our A&Es. A slide presented at the meeting showed we could end up without a full A&E at either hospital. The slide said that one emergency centre or specialist emergency centre is planned – but draft specifications from NHS England say that only specialist emergency centres provide full A&E care.
The delay to the public consultation is because the Clinical Commissioning Groups don’t know if the hospitals Trust will be financially viable in five years time and are waiting for it to produce a Five Year Financial Plan.
The Trust – along with half the Foundation Trusts in the country – is in deficit. It is under special measures from Monitor, the NHS competition enforcer and financial regulator. Monitor is telling it to make big spending cuts, since Foundation Trusts are not allowed to operate at a loss.
Waiting on the next Comprehensive Spending Review
In an extra whammy, CCGs’ Finance Officer Julie Lawreniuk told the joint Governing Bodies meeting today that Calderdale and Greater Huddersfield NHS as a whole is now predicted to be short of £155m by 2020, unless big cuts and changes are made.
Nationally, an annual £22bn funding gap is forecast for the NHS by 2020, unless massive “efficiency” savings can be made.
Ms Lawreniuk said,
“Half the Foundation Trusts are in deficit. What happens next depends on what’s in the next Comprehensive Spending Review. What money is coming into the NHS in the next three years? At the moment, the NHS is not sustainable.”
The Trust fell into deficit last year, as a result of what Monitor described as a “perfect storm”. This included:
- NHS funding since 2010 at below the rate of inflation – an effective funding cut;
- An impossible demand from the government for the Trust to make £20m efficiency cuts in 2014/15,
- The high cost of employing agency nurses to bring up numbers to safe staffing levels
- The high cost of the Calderdale Royal Hospital PFI contract, which eats up around 10% of the annual NHS budget for Calderdale. According to a Treasury spreadsheet, the PFI charges are predicted to cost the Trust £132m over the five years to 2020.
The Trust has just put out an invitation to Corporate Finance and Financial Strategy consultancies to tender for the job of producing a 5 Year Financial Plan for Monitor, to show that it is financially sustainable.
The Trust’s invitation to tender has gone out through Crown Commercial Services, which has a list of approved financial consultancy companies, including the usual suspects like Deloitte, Ernst & Young, KPMG, McKinsey etc.
The cost of this consultancy is not public knowledge.
The Trust’s intention is to have the consultant in place by October and the Five Year Financial Plan finished by December.
This means that January 2016 is the earliest date for consulting the public about the proposed hospital cuts and shift of hospital services into the community, known as Care Closer to Home (CC2H)
Effects of delaying public consultation
The Secretary of Calderdale 38 Degrees NHS Campaign, Rosemary Hedges, asked about the effects of delaying the public consultation, and in particular whether this would delay moving hospital services into the community. Dr Alan Brook, Chair of Calderdale CCG Governing Body, said,
“By the time the consultation is over, whichever the result, changes to the hospital which have already been agreed in outline form will be unavoidable and there’ll be no going back.
“While we’ve agreed clinical consensus on an optimal model, we don’t know if this is deliverable or when services will be delivered…
“The answer as to whether there will be a delay in CC2H, certainly the CC2H exists in different phases. Phase 1 – strengthening existing services – proceeds apace. But there are other items which will be dependent on a consultation on hospital services & they will be held back until after the consultation’s taken place. They are a reason for us giving this high priority and we’re very keen to proceed as quickly as we can.”
The NHS in Calderdale and Greater Huddersfield has been facing significant financial pressures since 2010. These financial pressures were a key reason for the proposed Right Care Right Time Right Place scheme, which was first announced in February 2014.
It’s proposal that only one hospital will provide acute and emergency services, while the other becomes a small planned care clinic, met with widespread and continued public protests.
The Right Care Right Time Right Place scheme is intended to stop the Calderdale and Greater Huddersfield NHS funding gap from opening up. It aims to reduce demand for costly acute and emergency hospital services and replace them with “Care Closer to Home” community services for frail elderly and chronically sick patients.
Care Closer to Home is “no panacea”, says Monitor
But Monitor – the NHS competition enforcer – has recently warned that schemes like this are not guaranteed to reduce costs, or demand for health services.
In its new guidance on cutting demand for NHS services – which was not mentioned at the meeting – Monitor says that:
“Our findings caution against expecting too much from a shift away from hospital settings; this is no panacea.
“Developing schemes to move healthcare closer to home should sit alongside processes and decision systems within acute hospitals.
“The schemes will need to work effectively with other initiatives designed to address shorter run challenges, such as measures to ease the flow of patients through acute hospitals.”
‘CCGs like rabbits caught in Monitor juggernaut headlights’
Monitor seems to have the whip hand over Calderdale and Huddersfield hospitals. Terry Hallworth, a member of the public from Huddersfield, said,
“Both CCGs are like rabbits caught in the headlights with the juggernaut of Monitor bearing down on them. All their plans and deliberations are meaningless and totally dependent on what Monitor decides about CHFT. And Monitor doesn’t give a damn about the CCGs, public or CHFT. They are concerned with one thing and one thing only. Money.”
Jen Mulcahy, the Right Care Right Time Right Place programme manager, said that one of the risks the CCGs faced was that CHFT would not be successful in securing central funding.
So it looks as if CHFT is looking for a bail out from the Department of Health.
Dr Judith Parker, from Greater Huddersfield CCG Governing Body, said that another risk was the increasing numbers of CHFT staff who say that the Trust is not a good place to work. There are problems employing mid-grade staff and high level staff are leaving.
Dr Rajesh Phatak, the secondary care specialist on the Calderdale CCG Governing Body, said that on top of that,
“We need to be mindful of national issues including the new doctors’ contracts and the 7 day working issue. As a governing body we have little influence on this, nor do CHFT.”
Unclear if there’ll be a proper A&E at either hospital
It’s unclear whether there will be a proper A&E at either Calderdale Royal Hospital or Huddersfield Royal Infirmary.
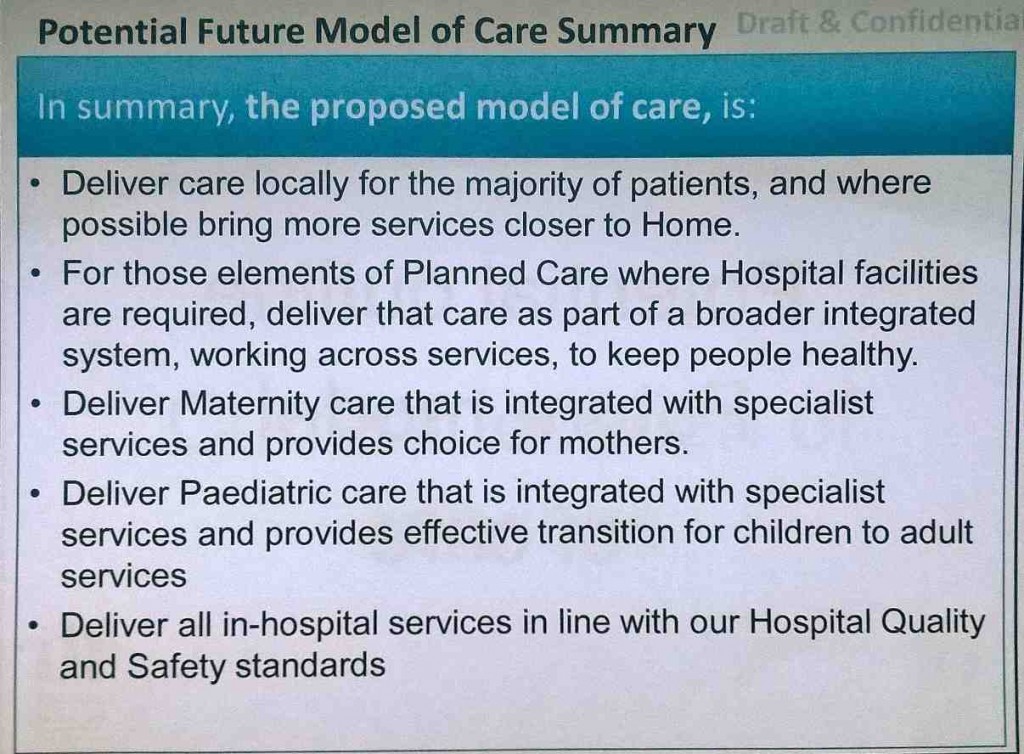
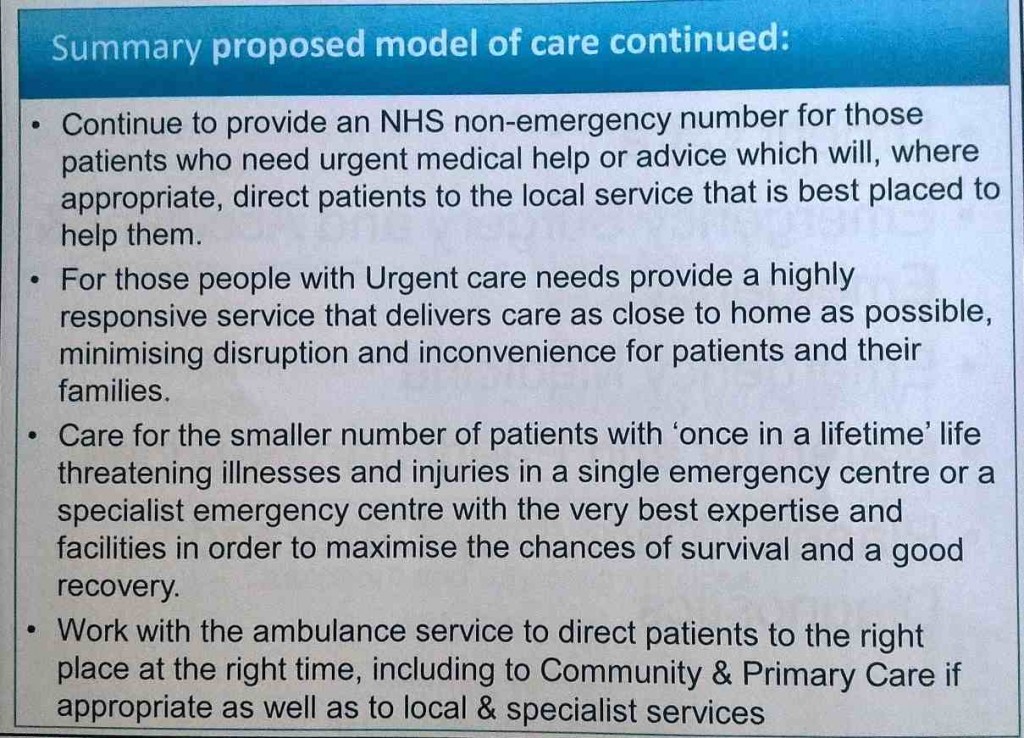
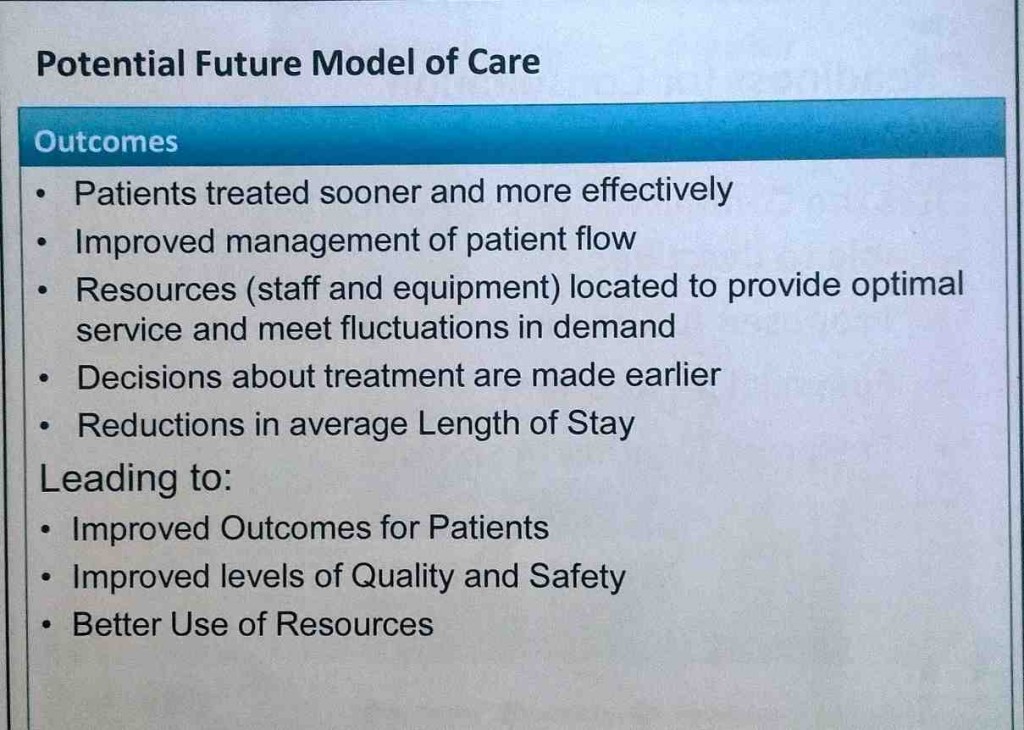
Jen Mulcahy’s presentation on the “Potential outline future model of care” included this:
NHS England’s August 2015 Draft Urgent and Emergency Care Facilities Specifications describe the following facilities:
- urgent care centres (UCCs),
- “Emergency Centres” and
- “Specialist Emergency Centres”.
The draft states that only Specialist Emergency Centres will provide the full back- up of the necessary consultant- led specialties to provide safe emergency care. The first two rely on being able to transport a seriously sick patient, by ambulance, to a hospital with a Specialist Emergency Centre.
Commenting after the meeting, Rosemary Hedges said,
“The proposed model of care is completely oblique and incomprehensible to any member of the public.”
Quality and safety versus the Monitor/CHFT financial plan
Dr Steven Cleasby, deputy chair of Calderdale CCG governing body, said,
“We’ve agreed on a clinical model of care but we’re not clear on the financial picture, apart from the £155m funding gap locally. Are we going to be in clearer position once the CHFT Five Year Financial Plan is in? And what weight regarding quality and safety competing with the financial case will be given, in deciding the location of the acute and planned care hospitals?”
Julie Lawreniuk explained that the Monitor/CHFT Five Year Plan will include a standard business case template that will evaluate the different elements and decide on the sites, including weighting factors.
Ms Lawreniuk said,
“We haven’t got the financial information yet. The CCG has to assure CHFT’s Five Year Financial Plan. What would happen to the CHFT estate? A lot of financial implications will be driven by the estate and the workforce. And can we say that the Five Year Financial Plan will be complete in 12 weeks?”
Dr Alan Brook said,
“The CCGs are not the agents of delay. We have to accommodate the clinical model within staff, finances and estates resources that are available.”
Matt Walsh, the Calderdale CCG Accountable Officer, said
“We need to watch the Monitor/CHFT Five Year Financial Plan and watch if it affects the clinical model.”
Paul Cooney, a member of Huddersfield Keep our NHS Public, said
“Clinical consensus has been reached – but another clinical model may come out of the Monitor/CHFT Five Year Financial Plan.”
Dr Brook said,
“The clinical decision is not dependent on the premise about the location of sites in one hospital or another – it’s not been developed in relation to one location or another.”
What next
At the end of the meeting, Carol McKenna, the Greater Huddersfield CCG Chief Officer, said that new risks had come through in the meeting that need to go into the CCGs’ timeline.
She said that on Monday 28 Sept the CCGs would give feedback on today’s meeting at a meeting with Monitor, CHFT and NHS England.
The next Calderdale CCG Governing Body meeting is on 8 October, 2pm, Shay Stadium, Halifax.
In mid October there is a Calderdale and Kirklees Joint Health Scrutiny Committee to discuss the consolidated timeline.
In view of the meeting’s discussion about the “engagement” process – not reported in this article – the CCGs will consider whether they need more engagement.
There may be another joint CCGs governing body meeting early in January 2016. This will depend on a review of today’s meeting.
Small prize for any member of the public who can make sense of these slides
Here are the CCGs’ slides about the proposed Right Care Right Time Right Place model of care, that Jen Mulcahy presented to the meeting. In the light of Rosemary Hedge’s comment about their incomprehensibility, Plain Speaker is offering a small prize to any member of the public who can make sense of them. Answers please: here.