Three NHS and social care organisations are planning the future of Calderdale’s mental health rehabilitation and recovery services.
Only two of them have explained their proposals to Councillors on Calderdale Council’s Adults Health and Social Care Scrutiny Panel. They want to cut beds and put patients into their own homes with unclear “support” in the community.
If you are affected by these proposals, please contact Plain Speaker.
Research shows that cutting mental health beds puts patients at increased risk of suicide.
Please demand of the Scrutiny Panel that Calderdale Council’s rehabilitation and recovery service and South West Yorkshire Partnership Foundation Trust (responsible for providing mental health services) each produce:
- the clinical evidence to justify closing 36 mental health rehabilitation and recovery beds and putting the rehabilitation and recovery service into the community
- impact assessments on patient care and staff.
Plans to cut recovery and rehabilitation beds and replace them by ‘flexible’ care in the community’ – whatever this might be
At the 8th September Scrutiny Panel meeting, the mental health Trust and the Council’s Rehabilitation and Recovery Service both presented proposals to cut mental health rehabilitation and recovery beds – although these vital beds are already in short supply.
Due to current bed shortages, 11 Calderdale patients are currently in rehab and recovery placements outside our district or in private facilities in Calderdale. A further 53 from Kirklees and Wakefield have also had to go outside their districts.
But John Keaveny from South West Yorkshire Partnership Foundation Trust (the mental health trust) outlined plans to close 3 SWYPFT rehabilitation and recovery units across Calderdale, Kirklees and Wakefield, with the loss of 56 beds between them.
The plan is replace them with one 20 bed unit to serve all three areas – without specifying where. This means losing a total of 36 beds.
This is despite the recent finding that:
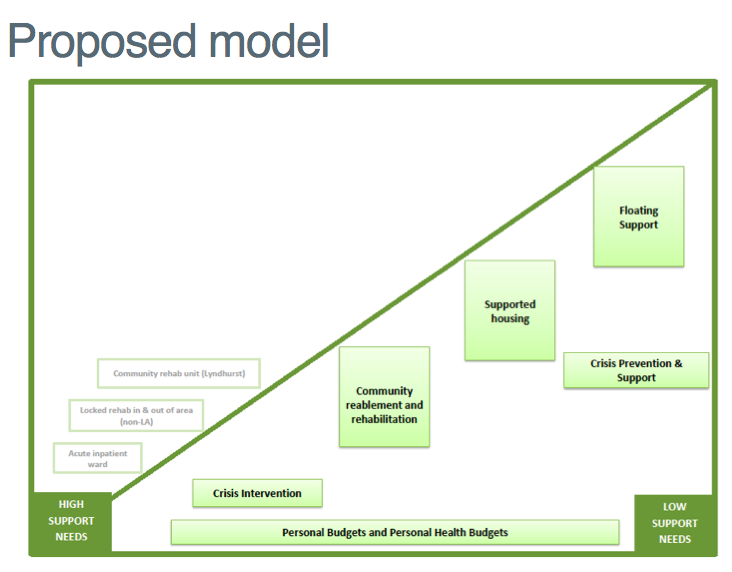
Both SWYPFT and the Council’s Rehabilitation and Recovery Service aim to move patients out of rehab and recovery accommodation into their own homes, supported by ‘a flexible community offer’ – whatever SWYPFT might mean by this jargon.
The Council proposes that mental health patients will pay for this community support using means-tested personal social care budgets and non-means tested personal health budgets.
Responding to this plan to move mental health patients out of rehabilitation and recovery accommodation into their own homes, a former NHS mental health worker said:
“People are only admitted to mental health beds under the Mental Health Act if they are at risk of harm to self and others, in other words suicidal. What this proposal is suggesting is that friends and family are to be on suicide watch. This is likely to have devastating effect on those who are trying to support someone with a Mental Health crisis. I would suggest that this will mean that people will stop being available to provide support and/or will need help from Mental Health services themselves.”
A new 20 bed unit for the whole of Calderdale, Kirklees and Wakefield is not care closer to home and could increase risk of suicide
At the moment there seems to be no public information about where South West Yorkshire Partnership Foundation Trust (SWYPFT) plans to put the new 20 bed unit.
So Plain Speaker asked SWYPFT about this. After initially replying with a load of spin about care at home, or closer to it, they eventually said:
“The proposals for a 20-bedded unit are based on our initial findings, which still need to be tested further and worked through with our commissioners and service users to make sure that they will fully meet people’s needs. After we have done this and should the plans still stand, we would then start to explore options for suitable premises. So at the moment, it’s too early to give a location I’m afraid. As and when the situation changes, please be assured that we’ll engage widely to seek people’s views.”
Wherever the new 20 bed unit might be, this doesn’t sound like care closer to home – it sounds like care a lot further away from home for many people.
Recent research has shown that sending mental health patients out of area increases the risk of suicide on discharge and should stop.
Questioned about this by Rosemary Hedges at Calderdale CCG’s Annual General Meeting on 10th September, the CCG’s Finance Officer Julie Lawreniuk said,
“There is no plan by the CCG to cut local bed numbers. Very few patients are cared for out of the area. Public Health is carrying out an audit of suicides in Calderdale.”
A former NHS mental health worker told Plain Speaker:
“Research shows that people recover best and quicker when in their own location, as family and friends can visit. Also people who have been admitted to residential stays have been triggered by an event; it’s been shown that moving people out of their location is detrimental to improvements in their mental health, as attachment problems are also then triggered.
How does the decrease in beds available from 56 beds to 20 beds equate to an improvement for service users?”
Is the “purchaser” at odds with the “provider”?
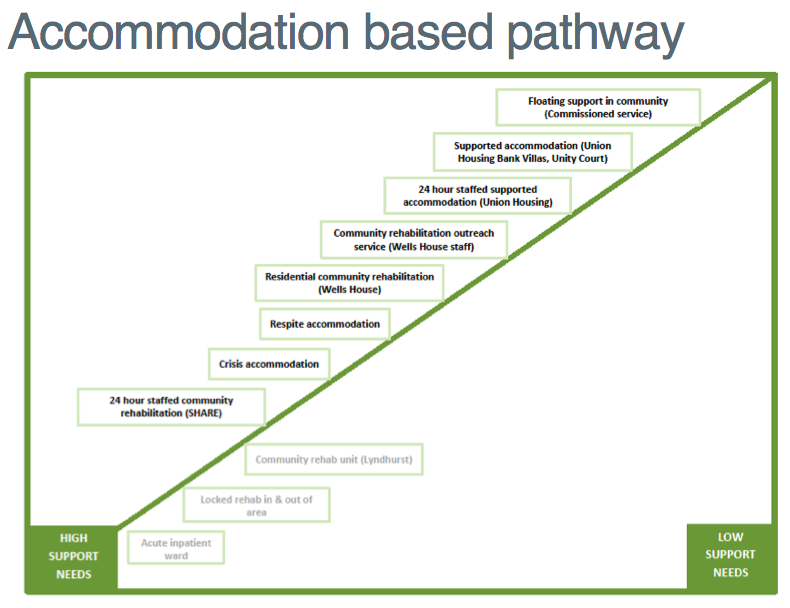
Lyndhurst – SWYPT’s 14 bed rehabilitation and recovery unit in Elland – is “out of scope” (not included) in the Council’s rehab and recovery plans, according to Libby Smith, the Council’s Rehab & Recovery Service manager.
This is because no one knows if Calderdale Clinical Commissioning Group – the “purchaser” of mental health services for the NHS – will agree with the proposed SWYPFT bed cuts in Calderdale, or buy beds in SWYPFT’s proposed new unit.
In response to a question from Rosemary Hedges at the Calderdale Clinical Commissioning Group AGM, the Finance Officer Julie Lawreniuk said:
“Rehabilitation and recovery beds in hospital are not effective, but they are effective in a community setting. The CCG has no plan to cut local bed numbers.”
As the CCG doesn’t want to cut local bed numbers, it seems unlikely to want SWYPFT to close Lyndhurst.
Libby Smith told Plain Speaker that she thinks the Lyndhurst unit may stay open for up to five years, but that uncertainty about the future of Lyndhurst means equal uncertainty about the future of Wells House (a SWYPFT residential community rehabilitation unit in Sowerby Bridge), and other Council rehabilitation and recovery accommodation. These currently house 59 people.
Libby Smith told Plain Speaker on 15th September,
“I don’t know about the future of Wells House, I don’t know if it will keep beds open, I don’t know what it will look like.
We had a workshop with stakeholders this morning and the next step is to draw up the services specification to go to Cabinet in November with proposals to consult.
We’re asking for permission to consult on the model and permission to implement. I don’t know what the politicians’ view is, if the Council should continue to provide rehabilitation and recovery services or just commission them.”
If SWYPFT were to close Lyndhurst regardless of the CCG’s plans, Calderdale CCG would probably aim to pay for private sector beds in Calderdale, such as Cygnet Lodge in Brighouse and Richmond Fellowship, Moorview.
The CCG already uses private beds in Calderdale when there are not enough SWYPFT and Council rehab and recovery beds. Use of these private beds is included in the figures for patients who are in “out of area” facilities.
Scrutiny Panel Councillors didn’t question drastic cut to beds or ask for good evidence to show it’s appropriate
Rosemary Hedges, who attended the 8 September Scrutiny Panel meeting, said,
“I’m not sure whether the Panel was aware that SWYPFT is proposing to cut the Rehabilitation and Recovery Beds across Calderdale, Kirklees and Wakefield from 56 to 20. I find it very strange that none of the members on the Panel questioned this drastic cut nor asked for good evidence to show that it is appropriate.
Rehabilitation and recovery is clearly a stage that starts before a person returns from inpatient treatment into the community, to live on their own. It appears that it is used for individuals who are returning to their locality after an in patient admission in an acute ward, often out of area and possibly of a secure nature, or in some instances it may be used to prevent or treat relapse (crisis/respite care). I find it very hard to believe that a population as large as SWYPFT’s can manage with only 20 beds of this kind across the whole of Calderdale, Kirklees and Wakefield.
I would suspect that financial restraints are driving these changes, rather than what is best for the patients. ‘Enhanced community care’ (which is often only one visit a day) is in no way an alternative to the 24 hour supervision and support that many of these individuals need on their pathway through the system.”
The first thing that the Scrutiny Panel should have asked for is the evidence data showing the clinical need to close rehab & recovery beds and replace them with care in the community.
And then they should have asked for the assessment of how the proposed changes will affect patients’ health, and staff working conditions and terms of employment.
What has the Scrutiny Panel decided?
Plain Speaker is confused over the outcome of the Scrutiny Panel meeting.
The Chair, Cllr Malcolm James, says he plans to discuss the SWYPFT plans with the scrutiny panel chairs in the other affected areas, since the plans are a significant variation to the existing service. He told Rosemary Hedges,
“The rather sudden nature of the proposal is a concern to us.”
But Libby Smith, the Council’s Rehabilitation and Recovery Service manager, said,
“We have agreement from the Scrutiny Panel to move ahead on the proposed model and to commit to working with SWYPFT to get there.”
It is hard to see how the Scrutiny Panel can have reached this agreement before the three Scrutiny Panel chairs have made up their minds about the SWYPFT plans. What is going on?
Resolve this mess – support the 2015 NHS Reinstatement Bill
The South West Yorkshire mental health Trust, Calderdale Council’s Rehabilitation and Recovery Service and Calderdale Clinical Commissioning Group all have administration, planning, procurement and contracting costs. These take money away from patient care and clinical staff salaries.
Surely this triplication and fragmentation is a waste of resources – particularly given the dire shortage of money in the NHS and social care, as a result of government underfunding.
It is also is a recipe for confusion, fragmentation, waste and lack of democratic accountability.
This is the direct result of Conservative, New Labour and Coalition governments’ successive moves to privatise the NHS and social care, by:
- splitting the previously integrated NHS into purchasers and providers,
- turning our hospitals into Foundation Trusts that are contractually obliged to make a profit, or face being closed down or taken over
- setting up local and national commissioning bodies that are required to buy services through competitive tenders that are open to private health companies as well as NHS ‘providers’.
All this while defunding the NHS through imposing huge “efficiency” cuts and flat funding, while also slashing Council health and social care spending. Not to mention the loss of at least £4.5bn/year to the costs of NHS marketisation and privatisation.
There is one clear way out of this mess, that damages patient care and staff working conditions and terms of employment.
This is to pass the 2015 NHS Reinstatement Bill, to restore the the system that once worked so well but now is crippled.
This Bill is simple and elegant in its vision of a fully restored, public health service that reinstates the NHS in order to maintain the health and wellbeing of an entire nation. It is designed to end the purchaser-provider split, reverse NHS privatisation and marketisation and resolve the PFI rip off.
The Bill includes a process for doing this without another top down reorganisation. It gives flexibility in how it would be implemented, led by local authorities and current bodies.
Its second reading is due on Friday 11 March 2016. Please ask your MP to vote for it, whatever their political party.
A 2013 YouGov poll found that 84% of the public want a fully nationalised, publicly owned and run NHS – and this includes 77% of Tory voters and supporters.
Updated 18 Sept 2015 with new information from SWYPFT.