Calderdale attracted national attention earlier this year as one of the worst places in the country for delays in hospital discharges of patients who are medically fit to leave, but still need nursing or social care afterwards.
Helen Barker, the hospital Trust’s new Interim Associate Director of Community Service and Operations, said that she is confident that the situation will be better in six months time, although she conceded,
“I’m a bit disappointed at this month’s performance”.
Together with Pippa Corner from Calderdale Council’s Adults Health and Social Care (AHSC) Directorate, Ms Barker attended the Council’s AHSC Scrutiny Panel on 11 August 2015 to explain the delays in discharging patients who need ongoing care once they leave hospital.
Pippa Corner told Councillors that of the June delays to discharge, 3 were due to social services and 28 delays were down to the NHS. Of these, 9 were people waiting for other health checks in hospital, for example waiting for continuing care assessment.
Helen Barker said the main cause of delays was internal communication in the hospital. Steps were being taken to remedy this.
“Patients have had too much choice”
Ms Barker said that patients have had too much choice to stay in acute beds when they were medically fit for discharge. She told Councillors:
“Patients have had the choice to stay in acute beds because they’ve refused other offers. We’ve now agreed a moving on process, with less choices for patients. Now they will have to go even if it’s into something transitional – which before, they haven’t done. They’ve tried to wait until they can get into a permanent home.
We will now get noise nationally because we’ve been lenient about patients being allowed to stay in an acute bed and they won’t be doing that now.”
Cllr Malcom James said,
“Patients have had too much choice, and now the discharge people are going to get heavy. Does ‘noise’ about this mean there’s a lack of capacity for people to go on somewhere else?”
Calderdale nursing home beds closed after failing Care Quality inspection- cost to hospital of opening extra beds is £0.42m in one month
No one at the Scrutiny Panel mentioned that the hospitals Trust has had to increase the number of beds and staff to make up for a number of intermediate care nursing beds that have been removed from the Calderdale community system until further notice, following inspection by the Care Quality Commission.
This has added to CHFT’s costs, particularly its pay costs, but Calderdale Clinical Commissioning Group (CCG) has refused to pay £0.42m invoices for additional bed and medical capacity in April. This is one of the causes of the dispute over the still-unsigned 2015-16 clinical services contract between Calderdale CCG and the hospitals Trust.
The Huddersfield Examiner (14/8/2015) reports that at the 28th July CHFT Board, Calderdale Councillor Bob Metcalfe, who represents the Council on the hospital Trust Board, said,
“The CQC regime standards are different and far more rigorous, and that’s right. Where quality isn’t right we have a duty to protect the vulnerable.”
Trust Chairman Andrew Haigh replied,
“It is right but it just puts pressure in the system which results on us.”
It seems odd that the Scrutiny Panel meeting failed to mention this elephant in the room.
And another elephant in the room was any consideration of the fact that a big part of the problem may well be Calderdale Council’s massive 2013 cuts to its Health and Social Care services, including decommissioning its intermediate nursing care home Heathy House and privatising/outsourcing rehabilitation and nursing care. Shouldn’t Councillors be talking about whether it’s time to bring these services back in house?
Problem looming with nursing care – “could get worse before it gets better”
Cllr Jayne Booth told Ms Corner and Ms Baker,
“Your challenges include nursing home capacity and packages of care, therapists etc. Without improving these, if it’s not there at the end, it’s not going to work. What are we going to do?”
Ms Baker said that, building on experience from elsewhere,
“We could have a virtual ward of 60 staffed beds, but beds in patients’ own home.
We are working on what we do about nursing home provision, what do we do about not-qualified nurse provision and replacing various therapists with one practitioner.”
Ms Corner said:
“There is a system-wide approach to building resilience in the nursing care market and nursing home sector, and continued work with the Care Quality Commission on the impact of regulatory actions.”
What does this mean?
Cllr Adam Wilkinson asked this question, but before Ms Corner had time to explain, Cllr Malcom James chipped in again with:
“Do we have a problem with nursing home capacity?”
Ms Corner said,
“In Calderdale we do have an issue we’re concerned about, and it could get worse before it gets better. We are trying to do work to bring more nursing homes into the market. The System Resilience Group’s working on it, but I’m not qualified to talk about this.”
Bev Maybury, Calderdale Council’s Director of ASHC, said there are 51 empty residential care beds, the residential care market is “flooded” and Calderdale could need less.
She added,
“There’s a small number of people who aren’t going to get nursing home beds – there are about four available now.
When you look at the reasons for delays to discharge, you have to look at what patients are waiting for. It’s not social care.
A problem’s looming with nursing care but you have to get it into perspective. Intermediate care, or convalescence, is necessary – don’t be in too much haste to move people through the system. You can spend a lot of time focussing on a small number of people.”
Iain Baines, Calderdale Council’s AHSC Head of Safeguarding and Quality, added:
“How many people in an acute hospital bed actually need a nursing home bed? Some will need nursing care, but a small number of people. The Care Quality regime has increased the number of homes that have got some action against them and that’s confused the picture.”
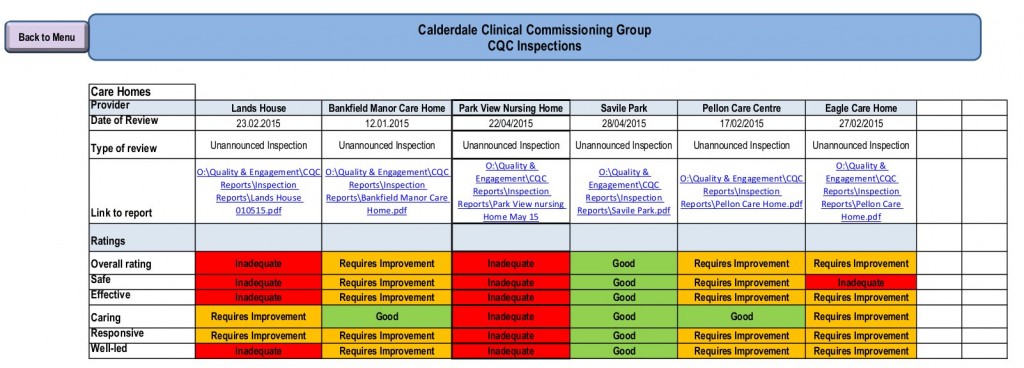
Calderdale Clinical Commissioning Group’s Quality and Safety Report to its 13 August 2015 Governing Body meeting shows the latest CQC inspection results for five Calderdale nursing homes and care homes. Park View Nursing Home is inadequate in every category. Lands House nursing home is inadequate in most categories and requires improvement in the rest.
Over-reporting
Pippa Corner and Helen Barker told the Scrutiny Panel that Calderdale had been over- reporting the numbers of patients stuck in hospital, as Calderdale set the clock for measuring the start of the delay too soon.
Pippa Corner said Calderdale’s reporting had been “over zealous” because they had started measuring delays to discharge from the time when the hospital patient was declared medically fit for discharge, instead of at the point when a multidisciplinary team agrees that the patient is ready for discharge.
The time between these two decisions varies, depending on the ward the patient is in. On high volume wards, the whole team communicates daily, so both decisions should be made on the same day. But if a social services referral is needed, this can take 2-3 days after the patient has been declared medically fit for discharge.
Ms Corner and Ms Barker told the Scrutiny Panel that in future the clock would be set ticking at the date when the multidisciplinary team agrees the patient is ready for discharge, and this would solve the problem of over-reporting.