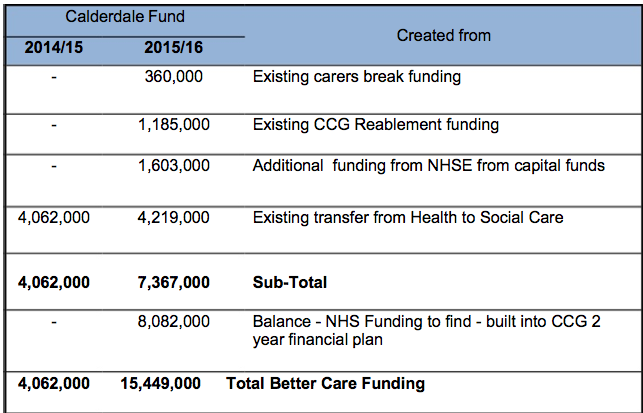
These are the questions Plain Speaker is asking Calderdale Adults Health and Social Care Scrutiny Panel at its meeting this evening. The Scrutiny Panel is scrutinising the Calderdale Better Care Fund plan to transfer money from the NHS to a pooled budget run by both Calderdale Council and Calderdale Clinical Commissioning Group.
1) Given the admitted lack of evidence that the Better Care Fund Plan is likely to reduce emergency and acute hospital admissions, how does it make sense for the Council to approve the Calderdale Better Care Fund plan, that takes £4m this year from the hospitals Trust – just as it is facing a deficit at the end of this financial year, and Monitor has increased the Trust’s risk rating that it will not continue to be a going concern?
This lack of evidence is borne out by:
- the admission of both Calderdale AHSC Directorate and Calderdale CCG, that there is little or no evidence that the BCF will work to reduce acute and emergency hospital admissions
- a National Audit Office Report that says “There is limited evidence that integrated care is cost-effective in sustainably reducing unplanned hospital admissions.”
- the NAO estimate that the Better Care Fund will only save £314 million – potentially leaving the NHS with significantly reduced budgets without reduced demand, after transferring nearly £2 billion of NHS funding to social care
- Margaret Hodge, Chair of the House of Commons Public Accounts Committee, who has said that “Planning for the Better Care Fund has been a shambles. The Fund is a complex and challenging initiative that clearly requires strong leadership and effective cross-Government working, both of which have been lacking.”
- A recent Nuffield Trust briefing (NHS hospitals under pressure: trends in acute activity up to 2022) said that plans to replace acute and emergency hospital services by care in the community (which is what is proposed in Calderdale and Huddersfield as well as across the rest of England) are not likely to work, given the evidence that “To date, attempts to reduce the numbers of people admitted to hospital through better preventative care in their communities have not been very successful on a large scale” ( p2) and “Current policy is aimed at cutting the number of emergency admissions by providing more, better services outside hospital that can either prevent the need for hospital admission or offer the same care but in different settings. This is a common theme in initiatives for more integrated services, including the government’s Better Care Fund. But there is little evidence that this can be achieved.(Bardsley and others, 2013).” (p11)
2)Please will the AHSC Scrutiny Panel ask Calderdale Clinical Commissioning Group the following questions?
Given the CHFT’s deteriorating financial situation and Monitor’s actions as outlined below:
- How is Calderdale CCG approaching the task of identifying the core package of essential services that would need maintaining if CHFT became unable to pay its debts?
- How are decisions about this core package of essential services split between the CCG and the management consultants appointed by Monitor
- How is Calderdale CCG working with CHFT to deal with its deteriorating finances and what measures does it advocate CHFT should take to sort out their financial position?
- If CHFT breaches its licence conditions at the end of the financial year and services have to be reduced, will Calderdale CCG consult the public about this, since it would amount to a service reconfiguration?
(At the 9 October CCG Governing Body meeting, I asked the above questions and was told by the Calderdale CCG Chief Officer Dr Walsh that the CCG would answer this question in writing within 4 weeks. The 4 weeks have come and gone without the CCG answering these questions.)
Update 21st November:
Calderdale CCG has now replied to my questions. Here is their answer:
Calderdale CCG response to questions about CHFT financial position
Background info about Monitor’s actions
Last September Monitor entered into a £210m, four year contract with ten consulting firms to develop plans for providers in “financial distress”.
Since the Health & Social Care Act (HSCA) 2012, Trusts have operated under a licence from Monitor that lists certain services as “mandatory” – they have to provide them, but only up until April 2016.
Between now and then, commissioners have been told by Monitor to identify services that would need maintaining if a foundation trust was unable to pay its debts.
Under Monitor’s contract with the management consultancy firms, the management consultants will in effect make many of the decisions about what are essential services that the Trusts would have to provide, in the event of failure.
Because of CHFT’s deteriorating finances Monitor sees an increased risk that the Trust will fail to to carry on as a going concern. It has increased the Continuity of Service Risk Rating (COSRR) to 2, put CHFT’s governance rating under review, and is requesting further information, before deciding next steps.
More info here
Plain Speaker’s report on the Calderdale Health and Wellbeing Board discussion of the Calderdale Better Care Fund plan to transfer money from the NHS to a pooled budget for Calderdale Council and Calderdale CCG is here.
Updated 11/11/14 to correct statement in Question 1 that the Better Care Fund will take £15m from the hospitals Trust in 2015-16. In fact the £15m is made up as follows: