Bootham Park Hospital was closed at the end of September 2015 on the sudden instruction of the Care Quality Commission, following their unannounced inspection five days before the contract for running the hospital was due to be taken up by Tees, Esk and Wear Valleys mental health trust.
The inspection was apparently triggered by whistle-blowing from a ward manager who used to work for the Care Quality Commission.
Despite massive public opposition to the hurried closure – and an assurance to the Care Quality Commission from the head of Tees, Esk and Wear Valleys mental health trust that they had £2m earmarked for fixing the maintenance problems that were the reason for closing Bootham Park Hospital – the Care Quality Commission refused to budge.
None of this story makes any obvious sense. So what’s been going on?
Do fast-revolving doors between key public organisations and private health sector companies create a shadow NHS, where decisions are made in the interests of profit not patients?
Trust’s Clinical Director is a business partner in AM Strategy Ltd – worth a small fortune from advising private companies how get access to NHS “market”
The Tees, Esk and Wear Valleys NHS Foundation Trust clinical director, Dr Ruth Briel, is the wife and business partner of former New Labour Health Secretary Alan Milburn – who, since leaving public office, has made a killing from advising private health companies on how to gain contracts from the NHS.
Together, Milburn and Friel own and are directors of AM Strategy Ltd, a company that gets its income primarily from consultancy to the private healthcare sector.
Set up in 2006, by 2013-14 the company had amassed assets of nearly £2m. This rose to £2.8m in 2014-15 before falling to £739K in 2015-16, due to outstanding payments to creditors of over £3m.
In 2013-14, when AM Strategy Ltd profits increased by £663,000, Milburn was working as a senior adviser to Bridgepoint Capital, a venture capital firm heavily involved in financing private health care companies moving into the NHS.
Milburn continues to work for Bridgepoint Capital as chairman of its European Advisory Board.
Bridgepoint Capital’s investments include Care UK – one of the biggest private health companies operating in the NHS. Its nationwide investment portfolio covers hospitals, GP surgeries and mental health centres, as well as £104m in NHS contracts since 2013 – including many of the 111 services that are going badly wrong.
Fox in charge of henhouse – Care UK boss sits on key NHS Improvement board, alongside TEWV clinical director
The Managing Director of Care UK, Jim Easton, sits on the Board of the NHS Improvement Faculty, alongside Dr Ruth Friel, the TEWV trust clinical director and business partner of Alan Milburn in AM Strategy Ltd.
The Care UK Managing Director’s presence on such a key Board of the NHS “market” competition regulator caused a bit of a scandal in May 2016, when the Faculty of Improvement was set up by NHS Improvement.
The stated aim of the Faculty of Improvement is to
“provide a hub of expertise which supports the NHS in England to find, share and embed improvements in the quality of healthcare people receive.”
It depends what you call improvements.
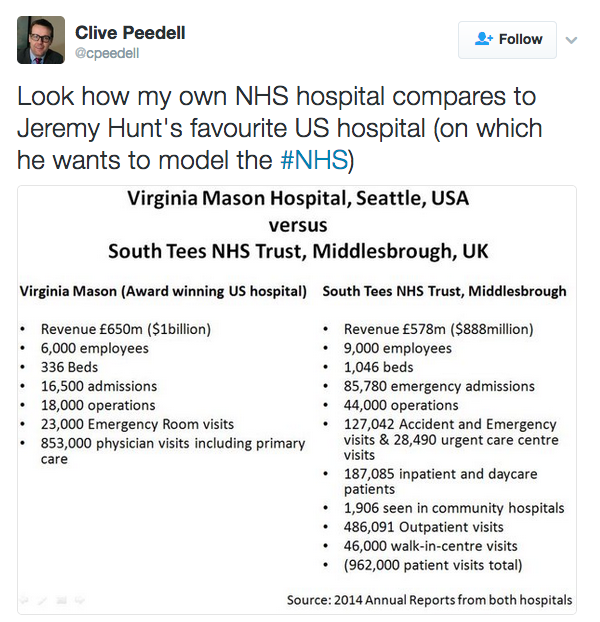
Under Dr Briel’s clinical direction, Tyne Esk and Wear Valley trust calls it adopting Toyota car manufacturing methods of “continuous improvement”, as well as “lean” methods from a private hospital in Seattle called Virginia Mason.
For this, Dr Briel and the TEWV mental health trust have received plaudits and the trust offers “improvement” guidance to other trusts.
But Virginia Mason isn’t all it’s cracked up to be.
Double standards apply: private American hospital, good – public NHS hospital, bad
In June 2016 – one year after NHS Improvement paid Virginia Mason £12.5m/year to tell five NHS trusts over five years how to introduce “lean techniques” that are meant to “create a sustainable culture of continuous improvement” – the USA’s Joint Commission (the country’s oldest and largest accrediting body in health care) denied Virginia Mason hospital full accreditation, after a unannounced review in May revealed non-compliance with 29 standards.
Among several crucial areas in which Virginia Mason didn’t meet standards, the Joint Commission found that the hospital was failing to inspect, test and maintain medical equipment; carry out fire drills; and provide an environment with no risk of “immediate threat to life.”
Following the unannounced inspection, Virginia Mason notified 650 patients dating back to 2011 that the hospital failed to properly screen clients for hepatitis B infections at an on-site kidney dialysis center.
That notice came more than a year after revelations that 39 people became ill, including 18 who died, during an outbreak of multidrug-resistant infections tied to contaminated medical scopes at Virginia Mason between 2012 and 2014.
You’d think the Joint Commission’s denial of full accreditation might cause NHS Improvement and Tees Esk and Wear Valleys mental health trust to review their embrace of Virginia Mason’s practices for improving patient safety and operational effectiveness.
But no. What is sauce for the Bootham Park Hospital goose is not sauce for the Virginia Mason Hospital gander. Double standards apply.
AM Strategy Ltd is paid by Lloyds Pharmacy and PricewaterhouseCoopers
As well as its links with Care UK through Bridgepoint Capital, Milburn and Briel’s company AM Strategy Ltd works with Lloyds Pharmacy; coincidentally or not, most TEWV hospitals have Lloyds pharmacies.
Another big AM Strategy Ltd client is PricewaterhouseCoopers, where Milburn chairs a board set up to expand the accountancy firm’s business interests in public and private health industries.
In 2013, Milburn said the health industry offered “strong opportunities” for growth for both PricewaterhouseCoopers and the wider economy.
In 2016 Milburn chaired a PricewaterhouseCoopers steering group that produced a report tacitly endorsing the current top – down NHS redisorganisation known as Sustainability and Transformation Plans; the report proposes changes to NHS England, NHS Improvement and the Department of Health in order to devolve the NHS to “local areas”.
This PricewaterhouseCoopers report, Redrawing the health and social care architecture, was supported by Jim Mackay, Head of NHS Improvement, where he is seconded from Northumbria NHS Trust – the first Trust to morph into an Accountable Care Organisation. This is an American import based on the Health Maintenance Organisations passed into law by President Nixon, on the grounds that they would increase health insurance company profits by delivering less care to patients.
NHS Improvement’s support for the PricewaterhouseCoopers report is unsurprising: the NHS Improvement Board Chair, Ed Smith, was formerly Global Assurance Chief Operating Officer and Strategy Chairman of PricewaterhouseCoopers, where he worked for 30 years.
PricewaterhouseCoopers is internal auditor of Care Quality Commission, whose chair previously worked for Pricewaterhouse Coopers
PricewaterhouseCoopers is also the internal auditor of the Care Quality Commission, where part of its role is to manage potential conflicts of interest.
In December 2015, the Care Quality Commission (CQC) appointed a new chair, Peter Wyman, who was accused by some MPs on the House of Commons Select Committee of having a conflict of interest because of his 40 year employment at PricewaterhouseCoopers (Pwc), until 2011.
Paula Sherriff, the Dewsbury MP, said ,
“PwC, where he was a partner for many years, is paid by the CQC as their auditor – ironically they even wrote the policy on conflicts of interests. And they also work for some of the companies that the CQC is meant to regulate…
The revolving door between private and public sectors leaves people wondering whether decisions are made in the interests of patients or profits.”
Campaigners point out that the revolving door extends to the Care Quality Commission and Bootham Park Hospital, where the maintenance issues were on a ward whose manager, Oliver Whyatt, was a former CQC inspector who whistle blew to the CQC.
Other Mental Health units have had far worse Care Quality Commission reports and they’ve not been closed. Tim Farron saved the Kentmere psychiatric ward in Westmoreland General Hospital from Care Quality Commission closure – at least until the Clinical Commissioning Group have carried out a public consultation on its future.
So what, exactly, has been going on in this Bootham Park Hospital game of cloak and dagger? Whose interests does its closure serve? Patients’ or profits’?


Seemingly the Health Foundation have been awarded a contract by Jeremy Hunt to source another contractor(Warwick Business School)at a cost of £400000, to evaluate whether another contractor Virginia Mason Institute is value for money or not ,wouldn”t 10 mins.on Google have found that.
Just a thought The Virginia Mason “Lean Medicine”theory is based on the Toyota car COs “Lean Production”methods did not Toyota Car Co.have to recall 11.5 million cars last year.
Thanks for info Mike, found the WBS link here Seems like a big fat waste of money to me. They’d do better to ask the Unions and their NHS members with experience of working under “lean” methods.